University of Michigan assistant professor of neurology Dr. Lisa McGinley sheds light on the current developments of stem cell therapies for Alzheimer’s.
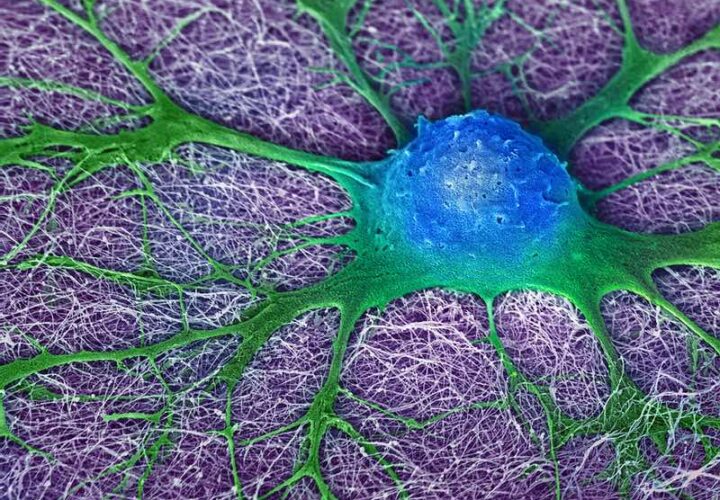
With the right signals, non-differentiated human cells called stem cells have the potential to divide and multiply into all different types of cells. Due to this superpower of versatility, scientists are exploring their therapeutic potential to replace damaged cells or tissue. Using stem cells in medical therapies has shown promise as a possible future treatment for neurological conditions like Amyotrophic Lateral Sclerosis (ALS), where stem cell therapies have shown in early studies to protect motor neurons and lengthen the lifespan of mice with the ALS gene, and are currently in stage 3 human clinical trials.
The results have also been a focus of great interest for Alzheimer’s researchers, who are working to crack the code on therapies for a disease that has been notoriously difficult to treat. This group includes University of Michigan Assistant Professor of Neurology Dr. Lisa McGinley. “The great thing about stem cells is that they can provide benefit in multiple ways, compared to drug therapies that typically target a single pathway,” she told Being Patient.
McGinley along with fellow University of Michigan co-investigators Dr. Eva Feldman and Dr. Geoffrey Murphy, is currently testing new therapies for AD in mice models. At the 2021 NIH Alzheimer’s Research Summit last month, McGinley shared encouraging data. “In our studies at the University of Michigan, we have found that transplanting our particular line of neural stem cells improves memory and learning in AD animal models,” she wrote to Being Patient in an email interview leading up to the NIH Summit.
In the long term, McGinley said the team is aiming to achieve similar results in humans, “with the hope of slowing or even stopping memory loss in these patients,” she said.
According to current research by the team, mice who received the stem cell therapies outperformed controls in learning curves and also demonstrated increased retention of learning. One group of mice had genes known as APP and PS1, which are both identified as causative genes for Alzheimer’s and heavily linked with early-onset Alzheimer’s. In addition to performing better, the group of APP/PS1 mice were also found to have reduced beta-amyloid plaque load – a known pathological feature of Alzheimer’s.
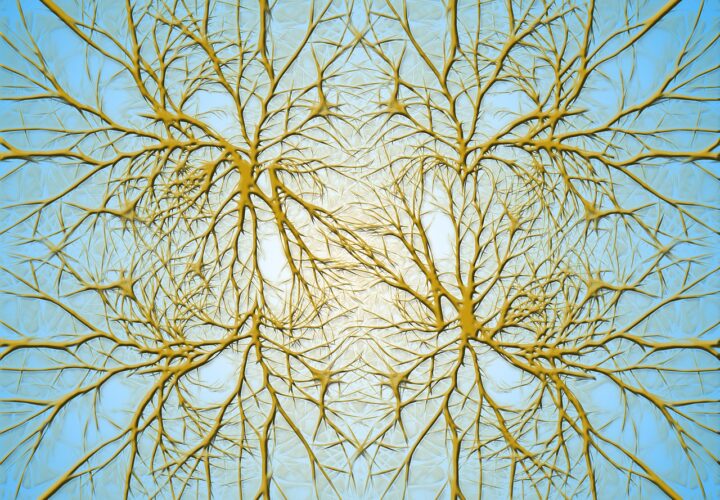
“Stem cells can work in several ways to improve brain function,” McGinley explained. “They can differentiate into neurons and they can form contacts with host neurons. They can also produce therapeutic factors and in this way reduce inflammation and provide support to existing cell populations in the brain. We are working hard to understand which of these actions are occurring and which have the greatest impact.”
In a human trial, stem cell treatments would be injected into the brain using MRI guidance. Although this may sound invasive, according to McGinley, there is a broad consensus that intra-cranial injections into the brain are safe, and accordingly, she said they are routinely used in various neurosurgical procedures. She added that the research team is collaborating with neurosurgeons at the University of Michigan in order to ensure the safety of these procedures.
While the results from animal models are promising, McGinley said there is still have some work to do to meet all the requirements necessary to obtain FDA approval for a clinical trial.” , “We are currently completing additional studies in animal models to help us understand how to effectively utilize stem cells in the brain, for instance what dose to use and when is the best time to administer the treatment,” she said.
As such, McGinley said that the time until these therapies become available on the mainstream market will still be a “number of years.”
Investigation continues into the safety and efficacy of these drugs in animal trials, using a variety of doses before testing can be done in human subjects.
In terms of roadblocks, other than funding, facilitating immunosuppression, which involves suppressing a recipients’ immune response to prevent rejection of the stem cells— is another challenge McGinley noted “but, we are learning from the world of organ transplants and developing new ways to prevent rejection of stem cell transplants, while minimizing side effects of immunosuppressive medications.”


I would volunteer for the stem cell therapy! Let me know when or if I might can get into this program!
I’m interstellar in this treatment for Parkinson’s disease! Have there been any tried and what were the results? I’m also interested in the cost and if insurance helps pay for it!
interested in stem cell peer review articles on latest breakthroughs!