'Where Is the Grandmother I Once Knew?': The side effects of common dementia drugs can make Alzheimer's patients' symptoms worse. I wondered if this was my grandmother's case. Here's what you need to know.
As a teenager, I would visit my grandmother over the summer and she was always the life of the party. She introduced me to James Brown, the Jackson Five and Anita Baker. Some summer nights, she cranked up the boombox and we would just dance.
“Life’s too short,” my grandmother used to say. I bragged about her to my friends. She was cool, energetic and vibrant—until her dementia began to progress.
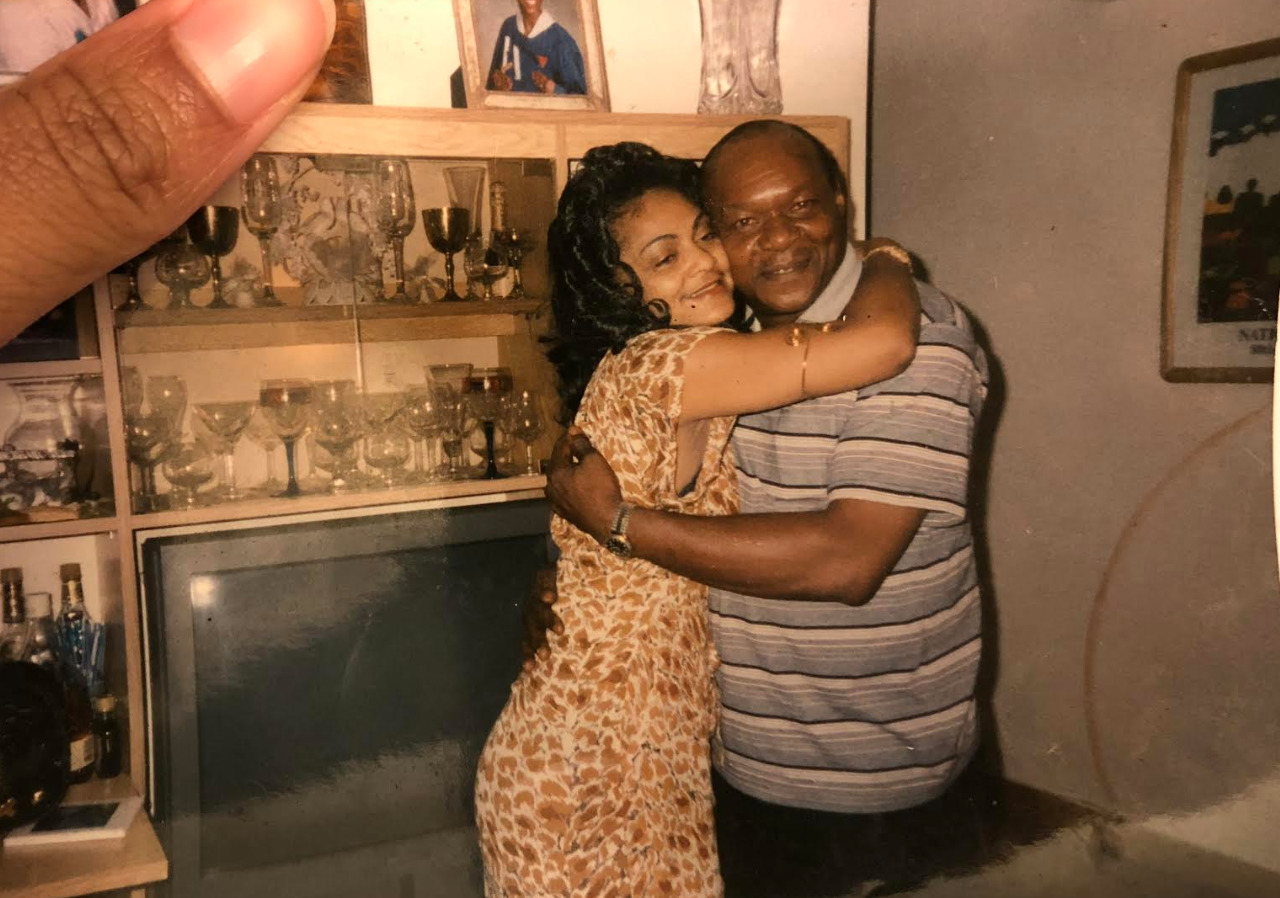
After my grandmother was diagnosed with young-onset dementia and cancer at the age of 60 three years ago, I started to accept that my grandmother would never again be the lively woman I once knew. Over the past year, she has become increasingly reserved—seemingly drifting off into another dimension whenever my mother, brother and I visit her.
When My Grandmother Was Admitted to a Facility, I No Longer Recognized Her
Last November, my grandmother was admitted to a rehabilitation facility after a bad fall. As a result, she stayed under attentive care for the entire month. During this time, a neuropsychologist prescribed her a dementia drug called memantine because she was having difficulty maintaining balance and swallowing. The drug, an NMDA receptor antagonist or type of anesthetic, is often prescribed to those with Alzheimer’s to temporarily alleviate confusion, and improve memory or the ability to complete daily tasks.
However, shortly after she started taking the dementia drug, she developed an inflamed sore throat—some people report a sore throat as a side effect of memantine—and was still having difficulty swallowing. My family had to remind my grandmother how to swallow because it was as if she had forgotten. Although her dementia may have been progressing, the dementia medication did not appear to improve her daily functioning.

While visiting my grandmother in rehab, I also noticed that she was no longer interactive. Despite being prescribed with medication that was supposed to improve her dementia symptoms, she had become quiet, childlike and distant. I started looking into the side effects of dementia drugs on patients.
Commonly Prescribed Dementia Drugs Offer Moderate Benefits
While one in three seniors passes away from Alzheimer’s disease or another type of dementia, there are currently no treatments that can stop or slow Alzheimer’s.
The FDA has approved three drugs that are meant to treat behavioral symptoms or memory issues linked to Alzheimer’s and some other forms of dementia: Razadyne (galantamine), Exelon (rivastigmine) and Aricept (donepezil). Drugs like Namenda (memantine) and Namzaric (memantine HCI and donepezil HCI) have also been approved to decrease dementia-like symptoms in those with moderate to severe Alzheimer’s. However, these drugs typically only mitigate symptoms for a short period of time.
While the dementia drugs may help patients initially, side effects can do more harm than good, according to Professor Clive Ballard, pro-vice chancellor and executive dean at the University of Exeter Medical School, who studies the impact of antipsychotic medication on dementia patients. (Memantine and the others drugs mentioned above are not antipsychotics.)
“There are benefits that take place over a 12-week period. But, they are very moderate benefits of improving certain symptoms, particularly aggression,” he said. “I think those benefits are outweighed by all of the other negative side effects for the vast majority of people—whether it’s very severe symptoms that cause distress or direct risk to themselves or others.”
Ballard said that antipsychotics in particular may cause dementia patients to develop other painful conditions.
“[Antipsychotics] can lead to parkinsonism, which leads to sores and walking problems. If you look across studies and combine them, you’ll see risk of chest infections and urinary tract infections as a result,” he said.
In addition to harmful side effects of these drugs, he said dementia patients often become heavily sedated from antipsychotics, causing them to become distant from their loved ones.
“They are more sedated [so] they sit down more, which can lead to chest infections because they are not walking around as much,” he said. “They are so sedated that they start to withdraw from people and they are not as interactive with other people as they used to be. So, they become less engaged and less active mentally as well as physically.”
I wondered: Were my grandmother’s personality changes because of her dementia, or the drugs she was on to treat her symptoms?
Initially, I thought my grandmother had only become distant and meek because of her dementia. Researchers suggest that early-onset dementia may cause mood changes, including apathy or a loss of interest in activities a person once enjoyed.
I continued to blame the sense of disconnection I felt from my grandmother on the disease—until I noticed something during a recent visit. My grandmother was hiding the memantine capsule her neuropsychologist prescribed her with on the tip of her tongue. Eventually, she agreed to swallow the medicine. Shortly after, the grandmother I knew, who had been fairly energetic before taking the pill, began to slip away.
Early one Saturday morning, my mother, brother and I arrived at my grandmother’s house in South Carolina. The woman I remembered—before dementia—came to greet us at the door. She smiled, then jokingly ignored my mother, rushing towards my brother and I, then asked, “How are my babies doing?”

My Grandmother Seemed to Be Experiencing Memantine Side Effects, Like Lethargy and Withdrawal
Later that evening, as my mother prompted my grandmother to take her scheduled dose of memantine, the upbeat grandmother who had greeted us began to fade away. After my grandmother placed the medication in her mouth, I realized something wasn’t right.
“Grandma, can you open your mouth, please?” I asked. The pill was still sitting on the tip of her tongue. “Grandma, you have to swallow the medicine, or the pills will burst. Are you having a hard time swallowing?” I added. “No, no, no, I will!” she said. Fifteen minutes later, the memantine still sat on the tip of her tongue, dissolving slowly. After 20 minutes, she eventually swallowed the pill with a large gulp of water, releasing a sigh.
Once the medicine was digested, she sat down on the couch, and my grandmother’s energy disappeared. She slipped into a state of sedation, staring with her eyes fixated on one spot for 20–30 minutes at a time. I asked, “Grandma, are you OK?” She only partially noticed that we were there, didn’t speak for the rest of the evening and eventually, she fell asleep. I realized she exhibited the same behaviors after taking memantine in the rehab facility.
Of course, my grandmother could have been experienced sundowning, a common condition that causes increased agitation in dementia patients during the later part of the day. But I wondered if the drugs might be exacerbating her confusion rather than helping her.
Side Effects of Dementia Drugs Can Heighten Dementia Symptoms, I Learned
Wesley Ely, M.D., a professor at Vanderbilt University School of Medicine, said that some dementia drugs, like antipsychotic drugs, lead to side effects like cognitive disruption that can heighten dementia symptoms.
“We found that [antipsychotics] are not beneficial. The benefits that you see with some antipsychotics can actually be a limitation in that person functionally interacting with their loved ones,” Ely said.
In addition to antipsychotics, Ely said that drugs like memantine can also cause dementia patients to become less alert than they were before taking the drug.
“Such drugs, while hopefully given to increase engagement, can have individual negative outcomes [including patients becoming more lethargic]. We find a great degree of interpersonal variability, which is one of the reasons why this class of drugs, while F.D.A. approved, has overall been a disappointment to most of the dementia community,” he said. “It’s a clarion call for all of us in medicine to act on our discontent. The future successes and improvements depend on us finding better treatments and, more importantly, prevention.”
I’m Not the Only One Who Suspected Memantine Was Making Her Worse
My grandmother’s caregiver also pointed out that memantine—which is not an antipsychotic—changed my grandmother’s personality.
“The memantine that your grandmother takes keeps her in a state of sedation. It’s like ADHD medicine for dementia patients,” she said. “It’s supposed to help slow down the disease’s progression, but instead, the medicine just holds her back.”
I wondered whether I was not only losing my grandmother to dementia, but also, to her medication. While dementia may have stripped her of the ability to verbally communicate fully, holding the medication on her tongue may have been her attempt at expressing awareness that the medicine would strip her of her personality.
Some patients who take memantine also report confusion, and though not as common, clumsiness or unsteadiness, trouble moving, feelings of sadness or emptiness and abnormal tiredness or weakness.
Alternatives to Antipsychotics and NMDA Receptor Antagonists
Paul Rosenberg, M.D., professor of psychiatry and behavioral sciences at Johns Hopkins University School of Medicine, researches depression and other neuropsychiatric symptoms in relation to Alzheimer’s disease. He said researchers have been focusing on social interaction as an alternative to drug interventions. However, he thinks funding is limited for researchers who want to focus on lifestyle interventions because drug companies in the U.S. make billions of dollars.
Social Interventions May Help Improve Dementia Symptoms
“We are trying to amp-up the interventions of home care, which is a non-drug intervention. In America, people are more willing to turn to drugs because American medicine does not pay for non-drug interventions,” he said. “One reason that my colleague is studying home care is to persuade Medicare that funding selected family training could be worth it.”
In other words, he hopes that someday, families can receive funding for training that will help them better understand how to notice any physical pain that may be causing their loved one to feel agitated, including chest pain or a urinary tract infection, before they need to turn to drugs that treat these behaviors.
Rosenberg said families should ask their doctor whether they can offer their loved one any non-drug interventions to treat dementia symptoms first and address any previous medical concerns that may interfere with medications they are given. Also, if a loved one is on multiple drugs, he said it’s important for families to ask the doctor if there are any drugs they can eliminate.
“Pleasant activities such as social interactions as presented in clinical trials show that there are benefits,” he said.
Antidepressants Can Help With Agitation and Anxiety
He adds that antipsychotics are typically used to treat behaviors that may be caused by dementia-like agitation, but they are not the safest option. Instead, he said selective serotonin reuptake inhibitors (SSRIs) that are marketed as antidepressants are a better alternative for treating anxiety.
“I use SSRI first and I keep antipsychotics in the background. We are trying to repurpose drugs that are already on the market today. Right now, we are doing a study on two drugs: lexapro and escitalopram—they are SSRIs. We are doing a pretty big nationwide study to determine if it works to treat agitation in Alzheimer’s disease.
Marijuana May Be a Safer Option Than Antipsychotics
In addition, his team is looking at how ingredients in marijuana that are part of certain drugs can help Alzheimer’s patients reduce agitation.
“I am also studying the drug THC—you heard it right. [These] drugs we feel can be safer than antipsychotics,” he said.
Lifestyle Interventions That Involve Exercise, Socialization and Brain Exercise
Professor Ballard is also working on a study called PROTECT which focuses on treating dementia symptoms without drugs.
“We encourage cognitive exercise, physical exercise and social activities to help promote healthy lifestyles for those with dementia. I find that other outlets such as activities and social outings are better for an individual and more effective.”
Being the Voice for My Grandmother
Many times, those living with dementia feel as if they have lost their voice. It’s important for caregivers to advocate for them and evaluate whether antipsychotics or NMDA receptor antagonists are really improving their quality of life.
Studies have found that some antipsychotics make no difference for delirium or dementia. In addition, a report found that many nursing homes in the U.S. prescribe antipsychotic drugs unnecessarily to about 179,000 patients per week. Researchers also believe that some painkillers could triple dementia patients’ negative side effects and alter their personality. Other studies have shown that benzodiazepines, a class of drugs that are prescribed to treat agitation in Alzheimer’s patients, could actually lead to an early death.
My grandmother is not gone. Like many others with dementia, she has difficulty communicating how she feels. Since she can’t always use her voice, I want to be that voice instead.


My mother was given Memantine. She was told that because she naturally had a low heart beat, it was the only dementia medication she could have. In fact at first we had to pay for it as it was not on the NICE register. She took it for 5 years I think but I really don’t know if it did any good. There certainly was no improvement. She fell whilst at home and broke her hip and later whilst in a care home, she fell and broke her pelvis. Her spell in hospital didn’t help at all. Her speech became less and less between 2013 and 2014 and she hasn’t spoken since 2015, just before having to move into a nursing home. She was able to sit upright but couldn’t co-ordinate with a frame so has had to be hoisted. She is doubly incontinent, food has to be puréed, she drinks through a straw and is totally immobile except that she does tap her toes to music. Everything, including feeding has had to be done for her since 2015 (but she’s still not ill enough for CHC!).
My mom has just been prescribed this for her mild dementia…. Her doctor believes it will help to slow down progression and maybe improve her short term memory loss. After reading your article I’m hesitant for her to start it.. Some of the mild side effects she already experiences without this drug ! She doesn’t need those to become worse.!! Thank you for sharing this article! I doubt I will let my mom take this! Not convinced this drug is good enough .
I hope your grandma is doing better these days!! What a sweet granddaughter you are!!!
Excellent article and thank you for writing it. Antipsychotics like Seroquel are an abomination to medicine and to dementia patients
as well. I begged doctors to stop prescribing to my Mom but they never would.
Thank you so much for sharing your experience. I looked up this topic because my mother was prescribed Namenda 6 weeks ago and her personality has already changed. We’re off to the neurologist Friday and I hope we’ll be getting her off this medication.