How is dementia diagnosed? Dr. Marwan Sabbagh, a neurologist at the Barrow Institute, discusses the ways doctors diagnose Alzheimer's and other neurodegenerative diseases.
Editor’s note: Dr. Marwan Sabbagh will join Being Patient again on September 19, 2023 to revisit this topic and discuss dementia misdiagnosis, why it’s so common, and what patients and doctors can do to ensure accuracy. Learn more and RSVP for free here.
Although the National Institute of Health has published medical reports on guidelines to diagnose Alzheimer’s disease, it can sometimes take years for patients to get an accurate diagnosis from their primary care doctors. Expensive scans or lumbar puncture tests are one way to confirm the presence of beta amyloid plaques or tau tangles in the brain, but those aren’t an option for many patients due to their high cost.
In 2017, Being Patient EIC Deborah Kan sat down with Dr. Marwan Sabbagh, a neurologist, researcher, and leading expert on the diagnosis of Alzheimer’s Disease and other forms of dementia at the Barrow Neurological Institute, where he is the director of the institute’s Neurological Institute Alzheimer’s Disease and Memory Disorders Division, to talk about the best way to determine if a patient is suffering from mild cognitive impairment or dementia.
Watch the video or read a transcript below of our conversation about the shortcomings of the conventional methods of diagnosing Alzheimer’s, how clinicians differentiate Alzheimer’s from other forms of dementias, and the early symptoms of Alzheimer’s.
Being Patient: There’s a lot of confusion over how you get diagnosed for Alzheimer’s disease. Previously, we’ve been told that a PET (positron emission tomography) scan or a spinal tap are the only conclusive ways to figure out whether there are plaques and tangles in your brain. Why is there so much confusion over diagnosing dementia?
Marwan Sabbagh: The historical, medical practice in the United States has been to take a diagnosis of exclusion. You have a medical history, a neurological exam, cognitive impairment, historically, and then you get a MRI to exclude brain tumors, masses, hydrocephalus, or stroke. You get a thyroid [exam] to exclude thyroid problems, and you get a B12 level [test] to exclude deficiencies in B12. The problem is that a diagnosis of exclusion is a
grossly inaccurate approach. The diagnostic accuracy, at best, is 75 percent.
Being Patient: What are some of the essential questions you need to ask and what are some of the essential things that primary care doctors should be looking at in order to determine whether or not this is Alzheimer’s dementia?
Marwan Sabbagh: I think doctors know how to do a mini-mental state exam – a MOCA, Montreal Cognitive Assessment. They know what to do but they don’t know what questions to ask on the front end, so I’ve been proposing a restructuring of the initial side of the consultation. There are structured interviews that are available now – the AD8, the AQ and the IQ code. These are caregiver informant-based interviews. Do they have this? Do they have that? Are they doing this?[These questions] inform the provider to say, “It’s time to look further.”
“The problem is that a diagnosis of exclusion is a
grossly inaccurate approach. The
diagnostic accuracy, at best, is 75 percent.”
The second thing I propose is that we need to look at aggregate risk analysis. There are now ways to say that the probability of Alzheimer dementia is very high if you are age 85, have a family history, female gender, hypertension and diabetes. You can come up with a score that says the probability of Alzheimer dementia is very high.
Being Patient: I want to talk a little bit now about different types of dementia and diagnosis – a number of patients say they were misdiagnosed and a pathologist we spoke to said that, through autopsy, he found that the majority of cases in his practice are being misdiagnosed. How do you tell if it is Alzheimer’s or another type of dementia?
Marwan Sabbagh: Pathologically pure Alzheimer’s without any other pathology is quite rare. It’s only like 33 to 40 percent. Most Alzheimer’s is mixed with something else – hippocampal sclerosis, vascular change, argyrophilic grain (disease,) or Lewy body. Pure disease of any type is quite uncommon. A lot of people have overlap but they look typically like Alzheimer’s dementia, so the clinical presentation and the pathological presentation don’t always align as much as you would think they would.
“Pathologically pure Alzheimer’s
without any other pathology is quite rare.”
As a clinician, I ask “What’s the clinical syndrome and how do we go about teasing it out to make sure we have the correct diagnosis?” You are absolutely right. People are grossly misdiagnosed. Lewy body is not detected often. Most of the other dementias are completely missed.
Being Patient: Does it matter to the patient in the end in terms of how they’re dealing, and coping, and engaging in maybe lifestyle treatments or medication?
Marwan Sabbagh: It does. It matters a lot. The reason it matters is lifestyle modifications, which are probably very good for brain wellness and prevention strategies in the Alzheimer’s spectrum from pre-symptomatic to the full dementia probably do not have as much data to support the recommendations in other dementias. Flatly, I don’t think there’s any shred of evidence that lifestyle recommendations would help another dementia like Lewy Body or frontotemporal dementia.
What You Need To Know
About Mild Cognitive Impairment:
Is It ‘Normal’ Aging, Or Possible
Early Signs of Alzheimer’s?
Being Patient: Is there a difference in diagnosing early onset versus dementia as Alzheimer’s in an elderly patient?
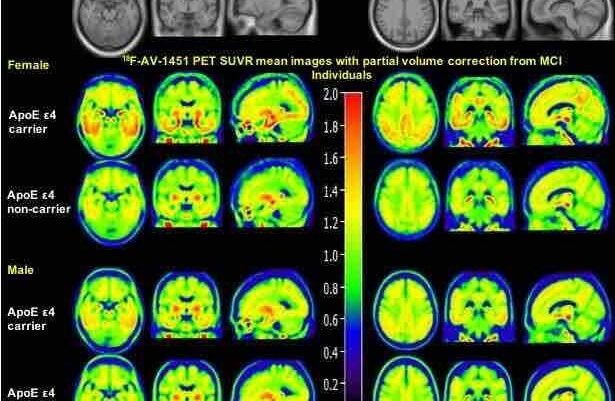
Marwan Sabbagh: In the way I approach it, yes. Most commonly, if it were a young person, early onset, I would do a spinal tap as my CSF (cerebrospinal fluid) confirmation to confirm the diagnosis. I tend to be a little bit more aggressive and invasive in what I do to diagnose my patients. Older patients, I might get a PET scan and, if it’s approved, I might get neuropsychological testing. I might get an ApoE genotype.
Being Patient: So many people now are impacted by this disease, a lot who are the children of a parent or a grandparent, and they want to know what are the early signs that they should look out for?
Marwan Sabbagh: You never misplaced things, now you’re misplacing things from time to time. You’re telling something repeatedly and you never did that before. These are the kinds of very subtle, very beginning things that would say [it’s] time to get an evaluation, especially if there’s a risk.
Being Patient: There are people who carry ApoE4, who have both one variant and are homozygous, and there are people who don’t, who end up getting Alzheimer’s. How much should that genetic profile enter into diagnosis?
Marwan Sabbagh: That’s controversial and I’m sure you’ve had different opinions from different doctors so I’m going to give you my perspective. I tend to be on the more progressive side of the discussion. In the clinical evaluation of my patients with mild cognitive impairment (MCI) due to Alzheimer’s or dementia due to Alzheimer’s, I frequently order an ApoE genotype. If they’re an ApoE4 carrier in the setting of MCI or dementia due to Alzheimer’s then the probability of Alzheimer’s pathology in the mix is very high.
I never order it for people who are asymptomatic, even if they have a family history. I agree with many in the field that it’s not inherently a diagnostic, it is simply a risk factor, but it’s a very rich risk factor because, if you are an ApoE4 carrier, the probability of having Alzheimer’s amyloid on your PET scan is very high. Some people are even proposing the idea of using it as a screening tool. Has this become common practice? The answer is absolutely no.
Being Patient: Once you give someone a diagnosis of Alzheimer’s dementia, do you believe the earlier you catch it the better off you are?
Marwan Sabbagh: I come from the school of thought that Alzheimer’s is a treatable disease. I am aggressive in treating my patients. I am proactive in addressing their healthcare needs, their family needs, their medication needs, their legal needs, and offering clinical trials as an added value to our clinical practice. Patients want that information. They’re seeking it. They’re craving it. They want it from a credible source.




T
Your two interviews, with Brad Dickerson and Marwan Sabbagh are very useful for somebody who has no knowledge of these conditions. Information is very clear.
Thank you Being Patient
Anne
Thanks so much Anne for your comment! It’s wonderful to know that Being Patient is succeeding in what we have set out to do – clarify the research and understanding of Alzheimer’s disease to the greater public. We appreciate you taking the time to give us feedback.
The questions asked were extremely on point, as were Dr. Sabbagh’s responses. Very informative!!
As a patient of Dr Sabbagh my loved ones and I appreciate his approach. I was diagnosed with behavioral variant FTD after a CFS determined no AD though PET scan and psych testing had suggest it.
Very good questions and answers. As a caregiver for my DW I felt the interview very refreshing. It is helpful to know what we don’t know as well as what we know about the disease. In our case our DX stopped with MCI of the alzheimer’s type. Since my DW is strongly in denial that is where all dx stopped. I have been reading comments on many of the dementia groups trying to fit her behavior into a specific type and have not had any success. I vascilitate from seeing many of the behaviors to seeing none. Her memory questions have been consistent and probably increased in frequency over the two and 1/2 years. I felt that she has shown improvement mostly because of changes I have made in my behavior as a caregiver.