Respiratory infections, including COVID-19 and also the common flu, more than double the risk of Parkinson’s, and more than triple the risk of Alzheimer’s, according to 2022 research.
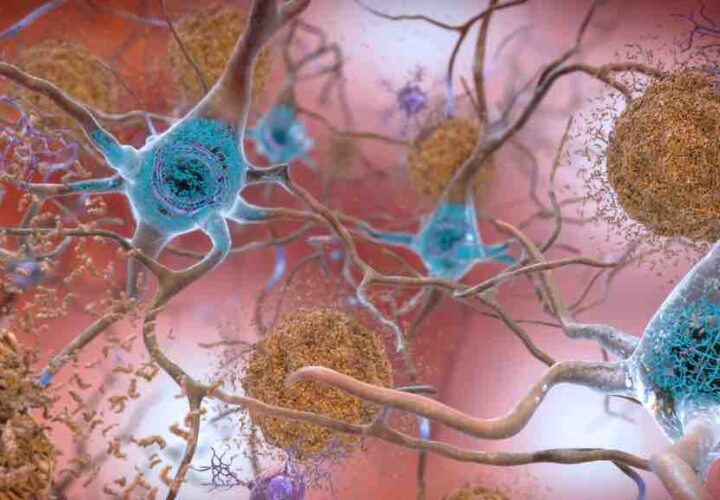
After coming down with the flu during the 1918 influenza pandemic, more than one million people developed a virus-induced form of Parkinson’s disease, with symptoms like confusion, fatigue and tremors. Now more than a century later, in the wake of the COVID-19 pandemic, scientists studying the causes of Alzheimer’s disease are exploring the link between viruses and the appearance of neurological diseases for answers.
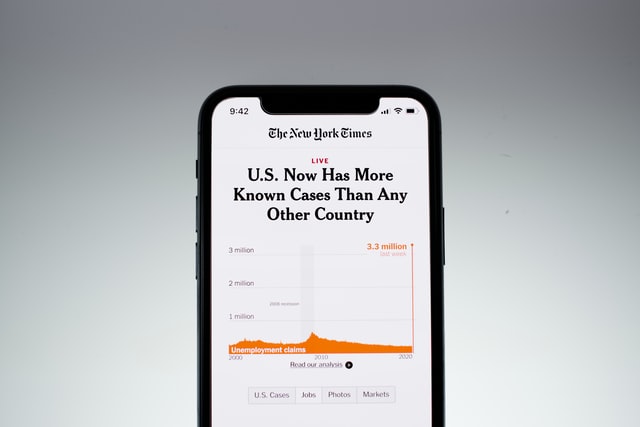
Researchers in Denmark tracked almost 3 million people between February 2020 and November 2021, to see whether COVID-19 infection increased the risk of being diagnosed with a neurological condition within the year. Compared to those who tested negative for COVID-19 in a hospital, people who tested positive were much more likely to be diagnosed with a neurological condition: Patients were at three-and-a-half times greater risk for Alzheimer’s, more than two-and-a-half times for Parkinson’s, almost three times for an ischemic stroke, and almost five times greater risk for an intracerebral hemorrhage.
Interestingly, looking at healthcare records, the researchers found these same levels of risk applied to older individuals who caught the common flu and bacterial-induced pneumonia. This builds on previous findings that flu vaccination reduced the risk of an Alzheimer’s diagnosis by as much as 40 percent.
People testing positive for COVID-19, however, had a more than one-and-a-half times higher risk of stroke if they were over the age of 80.
“We found support for an increased risk of being diagnosed with neurodegenerative and cerebrovascular disorders in COVID-19 positive compared to COVID-negative patients,” the study’s lead author, Dr. Pardis Zarifkar from the Rigshospitalet in Denmark said in a news release at the time of publication of the 2022 study. “Apart for ischemic stroke, most neurological disorders do not appear to be more frequent after COVID-19 than after influenza or community-acquired bacterial pneumonia.”
Links between a COVID respiratory infection and cognitive problems
In COVID survivors with persistent symptoms — known as “long COVID” — neurological symptoms tend to stick around. From brain fog, to neurologically linked sensory issues like loss of taste or smell, to sleep disturbances, anxiety, post-traumatic stress disorder (PTSD), to sudden strokes or lasting delirium, people have reported a range of neuropsychiatric symptoms linked to infection with the SARS-CoV-2 virus.
In spring of 2022, the most comprehensive ‘long COVID’ study to date found that cognitive decline associated with some cases of COVID-19 appeared to be equivalent to losing 10 IQ points. In “long-haul” patients, these symptoms persist for months. Evidence continues to mount indicating that the diseases do share the biomarkers of brain damage. This 2022 study found that the lasting impacts from COVID-19 on cognitive function — i.e. memory, attention, or problem solving — can result in cognitive impairment equivalent to suddenly aging 20 years, or losing 10 IQ points.
While the results were alarming, the study did not prove that COVID-19 leads to the development of Alzheimer’s or other neurological conditions. While people who had COVID have a higher risk of these diseases, there are other unmeasured factors that could be the trigger for both. For example, the people who tested positive for COVID-19 also carried a higher rate of cardiovascular disease, another risk factor for neurologic disease. This may mean that they were already more likely to be diagnosed with Alzheimer’s compared to people who tested negative for COVID-19.
The common flu appears to be just as closely linked to neurological disease as COVID is
Only future research can get to the bottom of why this relationship exists. But in a video interview, Zarifkar also noted that COVID-19 infection is unlikely to cause the development of Alzheimer’s or Parkinson’s on its own. The researchers didn’t find a significant difference between COVID-19’s effects and those of a flu infection: Both viruses lead to an increased risk of receiving an Alzheimer’s, Parkinson’s or stroke diagnosis.
“Most neurological disorders do not appear to be
more frequent after COVID-19 than after influenza
or community-acquired bacterial pneumonia.”
“It might have caused an acceleration, but it is unlikely that it has led to the development of neurodegenerative disease in one year,” she said, adding that so many people received a diagnosis after COVID-19 is because of an increased number of cognitive assessments, common at post-COVID-19 clinics. For other diseases like multiple sclerosis, Zarifkar added that researchers will need to study patients for much longer than one year.
Other factors the authors said they were unable to control for include socioeconomic status, lifestyle factors and length of hospital stay. The study’s results may also be biased, they noted, because it only included people who tested positive in a hospital setting. This excludes about four out of every five people who contracted COVID-19 in Denmark during that time but did not get tested in a hospital.
Scientists are exploring whether building up immunity through targeted Alzheimer’s vaccines could prevent or treat the disease.
UPDATED 10 April 2023: This June 2022 article was updated with new information to help our readers.