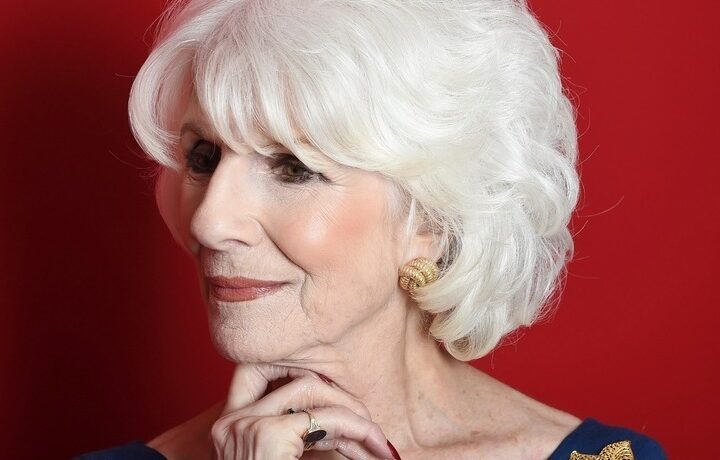
Kelly Bone lives with an early-onset Alzheimer’s diagnosis. She's fighting for the right to death with dignity.
For many contemplating end-of-life planning and the later stages of dementia and other cognitive disorders, euthanasia and assisted suicide remain contentious issues. While the right to die or “death with dignity” for Alzheimer’s and other neurodegenerative conditions is largely inaccessible in the United States, new developments in Switzerland and the Netherlands offer options for those committed to the idea.
- Different than assisted suicide, in which the individual administers a drug themselves, euthanasia is performed by a trained professional with explicit consent
- The nature of cognitive conditions makes it difficult to prove soundness of mind in making decisions related to euthanasia and assisted suicide
- While the ‘Death with Dignity’ movement is growing and nine states in the U.S. allow assisted suicide, laws exclude those with cognitive conditions
Being Patient spoke with Kelly Bone about her early-onset Alzheimer’s diagnosis and her fight for the right to death with dignity.
Confronting a Family History of Alzheimer’s
Being Patient: Why is the ‘Death with Dignity’ issue so important to you right now?
Kelly Bone: The reason it’s important to me is because I saw what my mother went through. She was diagnosed at 58 years old and ended up passing away from Alzheimer’s, and her death I felt was a very long and harrowing experience that I personally would not want to go through. I didn’t feel like it really allowed her to die with much dignity, even though she was in hospice. So, I’ve just decided that if there’s a way that I could possibly do it in a dignified forum, where I could go to another country or ideally to the United States, at the point in my life where my quality of life has diminished, I would like the opportunity to do so.
Being Patient: Since your mom had Alzheimer’s, do you have a familial link?
Kelly Bone: Yes, my mom had Alzheimer’s and my uncle had dementia, I had another great uncle who had dementia, my grandmother also, and then I have several great aunts and uncles who had it as well. So, it definitely does run in our family. I was very, very close to my mom, and my mom and I are almost like doppelgangers, you know I’m exactly like her.
We both had quite a bit of medical problems as well, so as we were going through it with her, I thought, “You know what, there’s a good chance I’m going to have it.” So when I had genetic testing done and saw that I have the ApoE4 gene, I decided to pursue it and have further testing done.
Why Choose Death Over Assisted Living?
Being Patient: A lot of people are really uncomfortable talking about this Alzheimer’s and end-of-life planning, people are either really for it or really against it. Tell us a little about your feelings on the topic.
Kelly Bone: I agree with you, I think it’s a very uncomfortable topic for people to talk about. When I talk about it with my friends and my family and stuff like that, a lot of them shy away from it, and some people just tell me, “I don’t agree with it” because of religious reasons. And I understand that. But for me it’s important because I have seen my mom and some other people that I know go through it.
For example, my mom lived in assisted living, and I ended up moving in and lived there for a while with her. So I saw firsthand what it was like to live in a memory care unit, I lived there full time for a while, and it’s not something I want to go through. I don’t feel that the people there have death with dignity. It was a beautiful facility that she was at, it had nothing to do with the facility. It’s just, not the way that I would like to go. And so, I’ve looked at different options.
I’m kind of going down a dual path right now if you will, where one of the things that I’m looking at is donating my brain to the Florida brain bank. I’m going on Monday to talk with the funeral home about how to do that, because I have to sign the paperwork while I’m healthy and all that, and I have to get all this testing done. So I’m looking at all that because there’s a chance that I’m not going to be able to do this in a dignified fashion, and I’m not the type of person who’s going to commit suicide. That’s not something I believe in.
I’d like to be able to do euthanasia, where I go on my own terms and I do it when my quality of life is diminished. So if I’m not able to do that, then I’ll go down the other path. So the other thing that I’m looking at is assisted living facilities. That would be the worst-case scenario for me would be to go into assisted living, I cannot imagine anything worse for me than to do that.
Being Patient: What is the difference between euthanasia and assisted living?
Kelly Bone: Assisted living would be where once I reach a point in my cognitive decline, my husband would put me into a home that would be a memory care unit for people who have Alzheimer’s, or dementia, or Parkinson’s disease. And I would go and stay there until the end of my life when they would bring in hospice so I could pass away at the home.
And then euthanasia would be where I would make arrangements with potentially another country, like you said the Netherlands, they allow euthanasia. Switzerland also does it, where you can do euthanasia and they do allow people with cognitive disorders. But Switzerland has much more stringent guidelines right now, and they do not allow people with advanced level cognitive disorders to pass away.
Being Patient: You would have to give permission for this to happen while you are still in an earlier stage of the disease, is that correct?
Kelly Bone: Yes, when I talked to the people in Switzerland about doing that, I would have to be able to sign the paperwork now, have my doctor sign off on it, get a second opinion saying that yes I have the Alzheimer’s diagnosis, we submit the paperwork to Switzerland, and then they would have their doctors verify it. I asked them, “Well, when would I do it? Would I do it later on in life?” Right now I’m at the very beginning of stage three of Alzheimer’s, and there’s seven stages, so personally I feel like I still have quite a bit of quality of life on the table.
However, what they told me was that no, I have to do it in Switzerland while I’m still totally cognitive. So that could mean that in the next year or two I’d have to go over there and allow them to administer the medication that will allow me to end my life. And that doesn’t really make sense for me.
So now, in the Netherlands they just passed a new law saying that they will allow people with advanced dementia to do assisted suicide or euthanasia as well. If you sign something now, and you get your doctors to sign off on it and things like that, they will potentially allow people to do that with advanced dementia. I would just like the opportunity to decide what I’d like to do. I don’t like the idea that I have to live with it, that I have to go into assisted living or stay at home and just diminish.
A Right to Death with Dignity
Being Patient: What does death with dignity mean, for you?
Kelly Bone: I know this is hard to believe, but I’ve had people tell me, even people who are police officers and things like that, you know what, you could always do it by doing this, and they tell me how to commit suicide. They give me suggestions of how to do it and things like that. To me, that is not dying with dignity. Going and doing it somewhere in my house all clandestine, not being able to say goodbye to my husband and leaving him with all that guilt, having him find the body and things like that, that to me is not a good way to go. It’s not fair to my family members.
I would like my family members, including my children, to be in on this and support me in the decision. At this point my family does support the decision, they just say, “Well, if that’s what you want to do,” and fortunately for me they were there when they say my mom pass away. They were there seeing her slowly diminish over a period of years. They understand why I’m saying the things that I do.
To me, that’s the difference. Not leaving the situation where all of my loved one’s walk in and I’ve taken an overdose of medication and I’m lying on the bed, or perhaps I didn’t die, or maybe I had a gun or something like that. To me, that is not dignified. Dignified is, I consciously made the decision, discussed it with my family members, I’ve discussed it with a doctor that’ll be administering it as well as my own doctors.
At some point, I’m going to move forward. And hopefully they’re going to support me, and hopefully my family members will be there for me when I do it. From what I understand it’s a fairly peaceful process, they administer the medication and half an hour later it stops your heart, and to me that’s a much more dignified and easy way to go when I’ve reached that point and that quality of life.
Being Patient: Do you have any reservations about going through with it?
Kelly Bone: I have cousins who have a lot of reservations about it, and they don’t think what I’m doing is appropriate. I don’t have any reservations about it because I’ve been a caregiver for people who have this condition, and I know what they go through. I’m a good person, and I’ve done a lot of good things for people in this life, and I’m doing a lot for the Alzheimer’s movement in trying to move the ball forward by doing a lot of fundraising and things like that.
I think God’s going to forgive me for this. I don’t think God is saying that he wants you to suffer, and I think God is an all-loving God and he’s going to have mercy on me if that’s the decision that I decide to make.
Edited for clarity





What ever your decision is Kelly, I’m sure it’s what YOU and YOUR family will agree on, I know you said a few days ago your Doctor was surprised how well you were doing….I believe in God, i’m praying for you, and hoping new medication will just around the corner for you my friend, you have the most positive attitude, God will keep watching over you <3
please be safe and know there are so many of us praying for you and your family <3
Thank you for speaking publicly about your life experiences and choices.
We need more open ended discussion about the realities that
people with dementia/alzheimers and their loved ones face ,
whether they realize or not.
Thank you for sharing your story. My maternal grandmother and paternal grandfather suffered from it. The hardest one was my grandpa. He helped raise me and I had just lost my dad. We had no idea his dementia/Alzheimer’s was already this bad. My dad had just passed away and my grandpa didn’t even realize that it was his oldest son who had passed away. I am not sure if I wanted to cry more for the loss of my dad or more because my grandpa no longer knew who my dad was. I would love people to be able to choose when they die when they have a terminal illness or dementia/Alzheimer’s. Too many people let their biases get in the way of decisions.
Thank you for this article. I was happy to hear that there is an underground movement working towards providing dementia patients with a peaceful death. I fully support that movement. I am doing my best to contact legislators in Illinois. I am more hopeful than I have been in the past. Thank you.
I was diagnosed with dementia in 2005 and had to quit work. In 2017 I was diagnosed with Alzheimer’s after having an MRI. I am fine now but I definitely want to die with dignity.