A large-scale study of 14,500 middle-aged women suggests that long-term antibiotic use could be linked to future brain health issues.
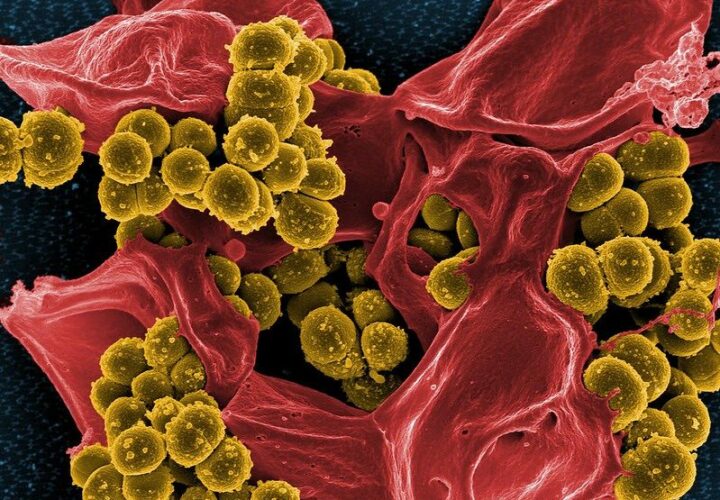
To treat many common bacterial infections, a short course of antibiotics is often prescribed. But in the case of chronic conditions — such as pneumonia or acne —long-term use may be required. As an unwanted side effect, even short courses of antibiotics disrupt the gut bacteria, and those play important roles in health and immunity. Could these disruptions affect cognitive function later in life?
Many researchers are focused on studying whether the gut microbiome could contribute to cognitive decline or even dementia. In one study of Alzheimer’s disease, individuals on a one-year course of antibiotics showed faster cognitive decline than those taking a placebo.
If killing some of the bacteria in the gut may worsen cognition, scientists wondered whether feeding these microbes specific fibers would have a positive effect. A seaweed-derived treatment in Phase 3 trials for Alzheimer’s may prove effective in treating the disease by feeding gut bacteria.
However, much of this research into gut bacteria-brain interactions is still fairly new, and many of the studies conducted so far have been small.
Now, a new study with thousands of participants, suggests a link between gut bacteria and healthy brain aging but from another angle: the study looked at long-term antibiotic use in middle-aged women and their likelihood of developing later-life cognitive decline.
In one study of Alzheimer’s disease, individuals on a
one-year course of antibiotics showed faster
cognitive decline than those taking a placebo.
More than 14,500 nurses were monitored at two-year intervals between 2014 and 2018. Taking into account long-term use of antibiotics — at least two months of usage — in the four years before the study. At each two-year interval, online tests were used to measure aspects of cognitive ability which included learning and working memory.
Seven years later, the researchers followed up with the nurses and found that long-term antibiotic use was associated with lower scores on these cognitive tests.
The results suggest there may be a link between gut health and cognitive aging, though there are several limitations. The study did not look at the impact of long-term antibiotics in men. It also did not collect information pertaining to which antibiotic an individual was taking.
Since the study is observational, it does not show that long-term use of antibiotics causes cognitive decline. And without collecting fecal samples, researchers can’t definitively correlate changes in gut bacteria quantity to changes in cognitive health.
Lynne Barker, associate professor at Sheffield Hallam University, who was not involved in the study, wrote of its findings: “The age of the participants is also an important factor, as the average age was 54 at the start of the study – which is the time most women experience menopause.”
Some women undergoing menopause may report brain fog, she noted. That means that the changes in cognitive decline could be partially attributed to hormonal changes which also influence the microbiome. Differences in hormone levels are also linked to some conditions requiring long-term courses of antibiotics such as acne.
“Menopause causes hormonal changes that can affect everything from how the immune system works, sleep quality, weight, blood pressure and even concentration and thinking,” she said.
While it isn’t definitive, this new study joins an ever-growing library of research indicating that the gut microbiome may play an important role in aging — and could have a direct influence on brain health. Luckily, many of the same foods that promote brain health are rich in dietary fibers and other nutrients that support gut bacteria.