One of a few kinds of gut bacteria singled out by scientists in a recent study appears to be associated with an 18-percent-higher chance of getting Alzheimer's disease.
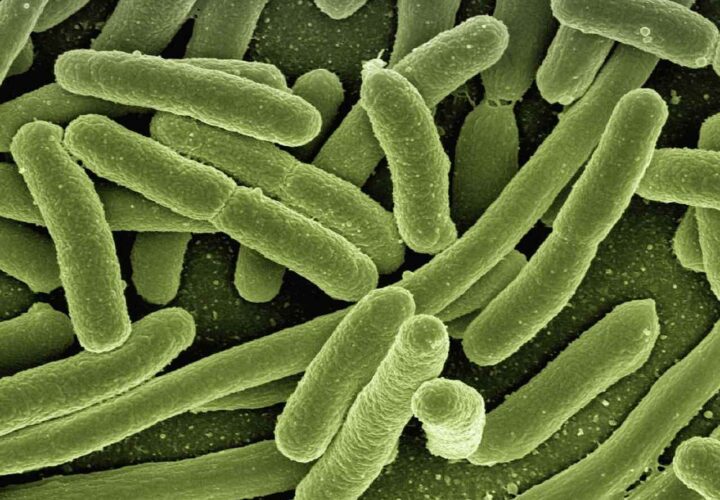
The human gut is home to trillions of microscopic organisms — collectively called the microbiome. The bacteria in the gut help digest food; they power the immune system, and they’ve been linked to many different health conditions — including neurodegenerative diseases like Alzheimer’s disease.
In 2021, scientists discovered that transplanting gut microbes from young mice could improve memory in older ones. Could it work in humans? Based on a new study that found some bacteria are linked to Alzheimer’s, researchers hope targeting these gut bacteria could treat Alzheimer’s symptoms.
In previous studies, scientists found that people with mild cognitive impairment and Alzheimer’s disease tend to have a different make-up of gut bacteria than people with healthy brains. In fact, there is such a strong link between the gut and the brain, it appears that even taking antibiotics — drugs that kill both good and bad gut bacteria — may increase the risk of cognitive decline.
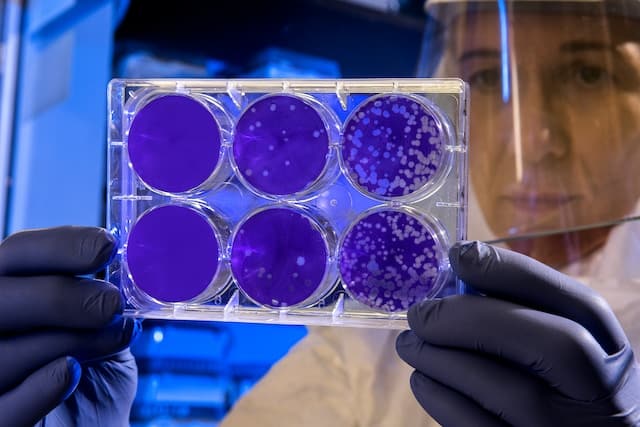
The new study published in the journal Scientific Reports analyzed the gut microbes of 2,077 people with Alzheimer’s and 2,081 healthy controls. People with Alzheimer’s had higher levels of certain types of gut bacteria. Some of these bacteria were also found in higher levels in the guts of people who had the Alzheimer’s gene, APOE4. This suggests a relationship between the Alzheimer’s gene and gut bacteria that could be contributing to Alzheimer’s
So, it follows, the researchers figure, that gut microbes could one day help doctors diagnose, and maybe even treat, Alzheimer’s and related forms of dementia.
The team wouldn’t be the first to suggest this approach. One drug, sodium oligomannate — or “the seaweed drug” — was developed to treat Alzheimer’s via the microbiome. But so far, scientists haven’t yet cracked the code: The seaweed’s drug Phase 3 clinical trials were halted in May 2022 due to financial challenges. But that’s just the beginning — researchers believe the way forward involves introducing beneficial bacteria into the gut to treat the disease.
Gut bacteria, Alzheimer’s, and APOE4
Everyone carries two copies of the APOE gene within their DNA, which encodes for a cholesterol-carrying protein called apolipoprotein E. Carrying a single copy of the APOE4 variant of this gene triples the risk of developing Alzheimer’s while carrying two copies could increase the risk up to twelve-fold. Could the effects of certain gut bacteria mediate the relationship between APOE4 and Alzheimer’s disease?
In the recent study, the researchers found that people with Alzheimer’s disease tended to have lower levels of six specific types of gut bacteria, suggesting they may be protective. Four other types of bacteria were present in higher levels compared to healthy controls, which may contribute to Alzheimer’s risk. One type of bacteria called Collinsella was associated with an 18-percent higher risk of Alzheimer’s disease.
The APOE4 gene is associated with a higher risk of Alzheimer’s disease, and levels of some gut bacteria were associated with carriers of this gene. Some but not all bacteria linked to Alzheimer’s were also linked to the APOE4 gene. What does this mean?
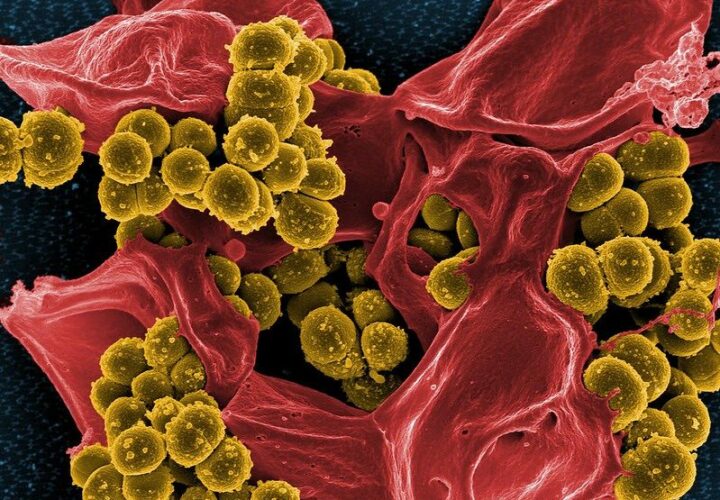
The levels of two microbes, Collinsella and Bacteroides, are higher in people with Alzheimer’s than in healthy controls. While there is no relationship between Bacteroides and people who carry the APOE4 gene, people with this gene had higher levels of Collinsella. It suggests that lowering the levels of Collinsella could be a targeted approach to reducing Alzheimer’s risk in APOE4 carriers. It could also mean that the interactions between Collinsella, the gut, and the rest of the body could fill in missing pieces of the APOE-Alzheimer’s puzzle.
Four types of gut bacteria were present in higher levels
compared to healthy controls. One type of bacteria
was associated with an 18-percent higher
risk of Alzheimer’s disease.
This is intriguing for sure — but the researchers emphasize that it’s pretty much impossible to draw any definitive conclusions at this point: There’s still too much we don’t yet understand about the microbiome. For example, while this study looked at the levels of certain gut bacteria, it didn’t assess the role that each of these bacteria are actually playing in the body. Researchers who look at active bacteria genes and other molecules they release have concluded that bacteria can be harmful or beneficial depending on their “function”; for example, gut bacteria that releases molecules to speed up bowel movement may be helpful during constipation but not so useful during diarrhea. Complicating matters further for gut bacteria researchers, the job a gut bacterium might do in the body can change over the course of the day, affected by factors like diet or exercise.
The chicken and the egg
This study suggests that some gut bacteria like Collinsella mediate the risk between Alzheimer’s and the APOE4 gene. This sets the stage for further research which will test if targeting this bacteria could reduce the risk of Alzheimer’s in people who carry this gene. But does APOE affect the gut microbes? Or do the gut microbes influence APOE? This is key to figuring out the elusive cause-and-effect relationship between the gut microbiome and other diseases and conditions, according to Jens Walter and other senior researchers at APC Microbiome Ireland.
Because risk factors for Alzheimer’s, like diet and exercise, have an effect on the microbiome, much more study is needed to get to the bottom of just what the relationship is, and how to control it, the researchers say.
In other words, people shouldn’t rush to the grocery store to load up on probiotics and other gut health supplements (which are unregulated, by the way). In the future, scientists do hope to harness the power of gut microbes to develop new diagnostics and treatments for Alzheimer’s, but in the meantime, science-backed, healthy lifestyle choices — like a Mediterranean-style diet, exercise, and addressing controllable health risk factors like smoking, hypertension, poor sleep and obesity — can keep the gut — and the brain — in shape.




From someone that carries the gene l find your articles extremely informative