YES, Medicare does now provide general coverage for amyloid PET scans for Alzheimer's diagnosis, following an October 2023 policy change.
As of a landmark policy change in October 2023, Medicare now covers PET scans to look for Alzheimer’s biomarker beta-amyloid in the brain for the general public. Up to this point, the Centers for Medicare & Medicaid Services (CMS) had refused to provide general Medicare coverage for Beta Amyloid Positron Emission Tomography scans (PET scans or amyloid PET scans for short), an often critical diagnostic tool in getting an accurate Alzheimer’s diagnosis and access to treatment. Now, a policy change — proposed in July 2023 — to undo restrictions on coverage of this procedure has been finalized. While Medicare coverage is now technically available for amyloid PET scans, this is a very recent change and patients should confirm with their doctors and plan providers that this is the case before the procedure.
Before this policy change, Medicare only covered one scan per patient’s lifetime within the context of an approved study. This requirement has been removed, meaning that people can receive one or more PET scans over their lifetime as part of the diagnostic process.
“Broader access to amyloid PET scans will enable earlier and more accurate diagnosis, and better care management,” Maria C. Carrillo, chief science officer of the Alzheimer’s Association said in a press release. “Their use can lead to better health outcomes for people living with Alzheimer’s or another dementia.”
Do you need a PET scan to diagnose Alzheimer’s?
These special brain scans, which can detect beta-amyloid, a key Alzheimer’s biomarker, in the brain, are also a key step in qualifying patients for Alzheimer’s clinical trials without which, new treatments and interventions would not be possible. And once those new treatments are on the market, doctors might require a PET scan to confirm Alzheimer’s before prescribing them.
For example, disease-modifying Alzheimer’s drug Leqembi (lecanemab) is now fully approved by the Food and Drug Administration — and covered by Medicare. But a PET scan is crucial in determining whether someone is eligible for and could benefit from drugs like Leqembi. These scans are expensive out of pocket — for many, completely unaffordable — which means that many Americans still haven’t been able to gain access to the only disease-modifying Alzheimer’s treatments out there.
Back in July, when this change was just proposed, Alzheimer’s Drug Discovery Foundation co-founder and Chief Science Officer Dr. Howard Fillit told Being Patient that its approval would be a landmark for Alzheimer’s care.
“Following Leqembi’s traditional FDA approval, it will be crucial to confirm the presence of amyloid plaques in the brain prior to and throughout administration to ensure that the right patients receive the drug and to monitor their response to treatment intending to remove plaques from the brain,” Fillit told Being Patient in July 2023. “Ceasing the once-per-lifetime limit that CMS currently has on amyloid-detecting PET scans would improve outcomes by making the tests more accessible, helping physicians to make definitive diagnoses of Alzheimer’s disease, and better informing anti-amyloid treatment decisions.”
There were a few exceptions already to the current lack of coverage: Medicare does cover PET scans only for people enrolling in certain clinical trials, and in that case, as Fillitt pointed out, for one amyloid PET scan per patient in a lifetime.)
Is a PET scan the only way to diagnose Alzheimer’s?
While Alzheimer’s diagnostic advances — from blood tests to retinal scans — are in the development pipeline, today there are ultimately only two reliable ways to go from cognitive symptoms to a definitive Alzheimer’s diagnosis.
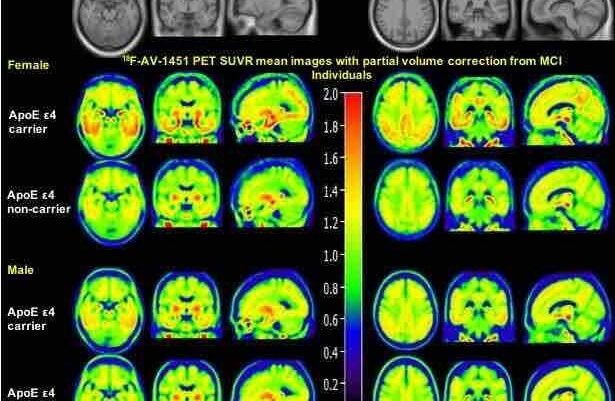
First, patients undergo a doctor’s appointment with a cognitive health specialist who considers a patient’s history and conducts a battery of cognitive tests. Then, there’s another step: looking for the presence of the disease’s key biomarker — beta-amyloid plaques in the brain — via a lumbar puncture or a PET scan, or a brain scan performed with positron emission tomography technology.
According to a 2020 Lancet study, approximately 35 percent of patients — those refusing or unable to undergo a lumbar puncture, and those with ambiguous symptoms — need an amyloid PET scan to receive a diagnosis.
What is a lumbar puncture and how is it relevant in diagnosing Alzheimer’s disease?
Lumbar punctures survey the fluid bathing the brain and spinal cord, called the cerebrospinal fluid (CSF), looks for fragments of brain plaques. PET scans involve injecting a safe radioactive marker into the bloodstream that binds to amyloid plaques in the brain. When the brain is scanned, these plaques “light up”. If someone receives a lumbar puncture and a PET scan, it is likely that the results will agree with each other. Sometimes, a PET scan however provides extra information that could correct a faulty diagnosis.
Some doctors require a PET scan and a lumbar puncture to diagnose Alzheimer’s
While lumbar punctures are covered by insurance, the CMS — the agency that decides what Medicare and Medicaid will cover — has refused general widespread federal insurance coverage of amyloid PET scans.
However, some doctors do still request that a PET scan be performed after a lumbar puncture, in cases where the results appear abnormal, and they want an additional set of data to confirm their diagnosis.
PET scans can ensure an accurate diagnosis
Even when the CMS denied general coverage of PET scans because they were not convinced it is “reasonable and necessary for [dementia] diagnosis or treatment,” they did write that PET scans were promising in two scenarios:
- “to exclude Alzheimer’s disease (AD) in narrowly defined and clinically difficult differential diagnoses, such as AD versus frontotemporal dementia,” and
- for selecting patients for clinical trials.
This ability to differentiate between dementias many different types is a critical advantage, when one in four patients living with dementia has been misdiagnosed. And there are many types of dementia that are difficult to distinguish from Alzheimer’s disease. Lewy body dementia is misdiagnosed 80 percent of the time, often mistaken for Alzheimer’s because the early symptoms are similar. If a lumbar puncture is looking for signs of beta-amyloid, they may well find it in these patients.
A misdiagnosis can have dire consequences. It means a patient isn’t getting access to the targeted care available for their particular disease. Meanwhile, they may be getting treatment for a disease they don’t have — and that can be dangerous. For example, while antipsychotic drugs are commonly prescribed for people with Alzheimer’s, they can cause adverse reactions in people with Lewy body dementia.
Alzheimer’s advocates have also expressed concerns that this refusal to cover a key procedure in dementia diagnosis and care for the low-income and/or aging Americans on CMS insurance programs has deepened racial and socioeconomic inequities in brain health treatment.

The science behind PET scans for dementia
A 2019 study called the IDEAS study followed launched in 2016. The research team sought to understand whether PET scans could change how doctors approach diagnosing and treating Alzheimer’s. They enrolled more 16,000 patients with dementia and mild cognitive impairment at 595 sites across the U.S. The CMS footed the bill for large portion of the bill for the study.
According to Gil Rabinovici, the first author on the IDEAS study and a professor at the UCSF Memory and Aging Center, their study showed that amyloid PET scans reduced hospitalization by 4.5 percent and provided a better diagnosis to 30 percent of the participants. It also showed that PET scans led to improved disease management for 60 percent of people, while also helping to correct misdiagnoses.
In the study, Rabinovici and team found that data from PET scans proved to influence how patients’ physicians referred them to clinical trials — one of the only pathways of access to cutting-edge treatments.
PET scan results also appeared to influence what doctors prescribed to patients. For people with mild cognitive impairment, doctors who confirmed that a patient had the amyloid plaques doubled their Alzheimer’s drug prescriptions: 40 percent prior to imaging rose to 82 percent after imaging. For patients with dementia, PET scans convinced doctors to up their Alzheimer’s prescriptions of drugs like Aricept to 91 percent from 63 percent.
About a third of patients previously diagnosed with Alzheimer’s were able to rule out the disease based on a lack of amyloid buildup. Half of patients who had not been diagnosed with Alzheimer’s received a new diagnosis based on the PET scan.
This study is just the tip of the iceberg when it comes to evidence that PET scans are critical to Alzheimer’s care.
“Beyond the IDEAS study, at least 30 published studies involving more than 4,000 patients have reviewed the utility of beta-amyloid imaging for the diagnostic assessment of patients evaluated for cognitive impairment in memory clinics,” William T. Thorwarth, CEO of the American College for Radiology wrote in a letter to the CMS on behalf of more than 40,000 radiologists.
“Beta amyloid PET contributes to diagnostic revisions in approximately 30 percent of patients,” he added, so without access to a PET scan, a large number of patients don’t have access to an accurate diagnosis.
Additional reporting by Simon Spichak
UPDATED 19 July 2:07 P.M. ET: A quote from Dr. Howard Fillitt at ADDF, received after the time of publication, was added upon receipt to provide more insight for our readers.
UPDATED 15 November 9:59 A.M. ET: This article was updated to confirm that the CMS does now cover amyloid PET brain scans for Medicare patients in the general public seeking an dementia diagnosis.


Re: CMS refusing to cover PET scans, the scans are expensive and Medicare is losing money with Medicare Advantage plans. Perhaps the CEOs of those companies that are overbilling Medicare could pay for said scans out of their ill-gotten gains.
I apologize for my crankiness. I’ve had 3 family members with Alzheimer’s.
This is a GREAT point, Sue.
What is the better diagnostic tool for the discovery of amyloid deposits – MRI or PET scan?
What is the cost differential?
MRI cannot detect amyloid. PET can but only recently was approved by insurance if you are taking any of the new monoclonal antibody drugs coming to market. Blood tests are coming to market and being used by some practitioners. These are a cheaper alternative to scans.
MRI cannot detect amyloid. PET can but only recently was approved by Medicare if you are taking any of the new monoclonal antibody drugs coming to market. Blood tests are coming to market and being used by some practitioners. These are a cheaper alternative to scans.