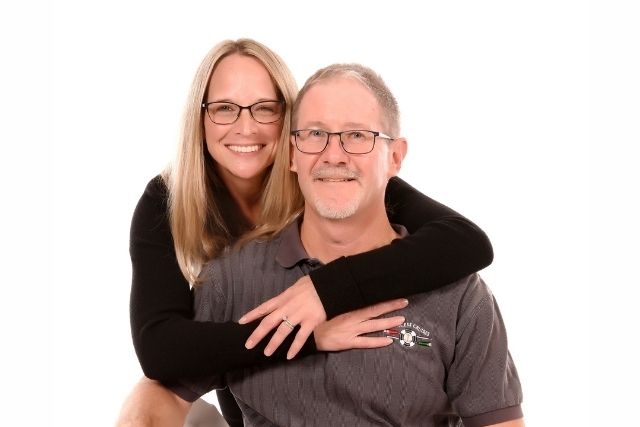
Scott Berkheiser was diagnosed with early-onset Alzheimer’s at age 56. That hasn’t stopped him from competing in IRONMAN races and advocating for dementia awareness.
Endurance athlete and former aerospace engineer Scott Berkheiser was diagnosed with early-onset Alzheimer’s disease at age 56, after years of unexplained symptoms and a misdiagnosis of ADHD. Now, even as he undergoes treatment, he continues to train for and compete in IRONMAN races.
Before his diagnosis, Berkheiser spent nearly two decades as an engineer at Lockheed Martin working on stealth fighter jets. In his personal life, he built a reputation for pushing physical limits, earning a national go-karting title and completing three full and 10 half IRONMAN races — one of them after his diagnosis. Now on a treatment regimen of Leqembi, Berkheiser is determined to keep moving forward, with plans to race again later this year.
In this conversation with Being Patient’s Mark Niu, Berkheiser shares how he continues to defy expectations, not only by competing in IRONMAN triathlons but by becoming a vocal advocate for Alzheimer’s awareness. Joined by his wife Kris, who now plays an essential role in his care and training support, Scott Berkheiser discusses navigating a life-changing diagnosis, finding strength through movement, and the hope that Leqembi offers in slowing disease progression.
Being Patient: For amateur athletes out there, tell me what completing an IRONMAN encompasses.
Scott Berkheiser: You start off [with] a 2.4-mile swim, a 112-mile bike ride, and then a 26.2-mile run.
Being Patient: And you have done how many?
Scott Berkheiser: I’ve done three full-distance IRONMANs and 10 half-IRONMAN distances.
Being Patient: It was about two years ago when you were diagnosed with Alzheimer’s. How did your Alzheimer’s diagnosis come about? What were the symptoms?
Scott Berkheiser: My brain was always my biggest asset in my career and everything else. My memory recall was good. I wasn’t the smartest person, but my logical thinking was good. And I noticed it started to slip a little bit. I mentioned it to our primary care doctor, and after I said it at a couple of appointments, they said maybe we should send you to the neurologist and get checked.
At that point, I don’t think other people were noticing it except [for] me, things that I should have remembered, I was starting to struggle [with] a little bit. I went to the neurologist, did a bunch of tests, [and they] basically diagnosed me with ADD. I was speechless that that was the answer. I kind of just shrugged my shoulders and moved on. And maybe 18 months to two years later, I still noticed it, but coworkers were starting to notice too. We’d be doing something and I would say something and they’d be like, “Scott, we just talked about that.”
My memory was so good I relied on it too much, so when I started to have some decline it became noticeable to me. For instance, when I was sitting in a meeting, I would take notes just by putting two or three words for something, just enough to jog my memory.
I was getting to the point where after a meeting, a day or two later, I’d be going through my notes, and I’d be scratching my head, saying, “What exactly did [I write]? What did that mean?” So I started noticing that. And again, people I worked with sort of noticed, but nothing major. They weren’t concerned, they just thought, “He’s getting older.” But that eventually led me to go back to the neurologist because I was feeling that I wasn’t at the top of my game. That time we went through the whole series of tests, including an MRI and the spinal fluid test, which is one of the confirmations of whether you have Alzheimer’s or not. It turned out that it was positive for Alzheimer’s disease.
Being Patient: Kris, were you noticing things at this time?
Kris Berkheiser: When he had first gone to the neurologist in the beginning, it was more [because of] what he was noticing. He would point out, “I walked in the room and needed to do something but forgot what it was.” And I was like, well, I do that all the time. I guess at that stage, I didn’t think there was really anything wrong. But as a couple of years went by, I did start to notice different things that were uncharacteristic for Scott.
Being Patient: And Scott, your parents had Alzheimer’s, is that correct?
Scott Berkheiser: My mother did, and her father, so my [grandfather].
Being Patient: So you helped your mother and had some understanding of what it was like?
Scott Berkheiser: Yeah, a little bit. She was older [when she got it], so we cared for her for about six months to a year. And then [she] had to go into a nursing home. That was really eye-opening when she came to live with us because she was the sweetest woman you could ever meet. I never heard her curse. When she was in the mid-later stages of Alzheimer’s, she sounded like a sailor at times. Where did this come from? It was shocking to see how it changes someone’s personality. She declined fairly rapidly. Shortly after she passed away, her dad, who was a police officer, had to retire because of issues he was having. And he declined very quickly after he stopped working.
Being Patient: What treatment are you getting today?
Scott Berkheiser: I take Leqembi. It’s an infusion that I get every two weeks. After a certain amount of time, you go to one a month instead of two a month. So I’m coming up on that shortly, which will be a little easier.
Kris Berkheiser: And it’s a [one-hour] infusion.
Being Patient: How’s the feeling of taking that drug? Is it difficult to tell its effects?
Scott Berkheiser: It is difficult to tell, but I truly believe it’s working. For one, every time I go to the neurologist, I do a cognitive test in the office. Up until my last visit, I got the exact same score every time. That’s what Leqembi is supposed to do. It’s supposed to slow the progression down. Going 18 months with no decline based on the test scores, and then maybe just starting to go down, in my belief, it’s doing what the drug’s supposed to do, slow the decline down.
Kris Berkheiser: We can quantify it with actual results. Before he started Leqembi, about two months before he started the infusions, he did all the finances, balancing everything in a spreadsheet.
“That’s what Leqembi is supposed to do.
It’s supposed to slow the progression down.
Going 18 months with no decline based on
the test scores, and then maybe just starting to go down,
in my belief, it’s doing what the drug’s
supposed to do, slow the decline down.”
He was having trouble with it, so I would come in and help. And then he gave up and he just said, “I can’t do it anymore.” Which was fine, I have a finance background, so it was easy to take it over, but it was heartbreaking for him. He started the infusions on December 18, 2023, and by mid-February, he wanted to try and do [the spreadsheets] again. He’s been doing it ever since.
Being Patient: Has it affected your training for the half marathons?
Scott Berkheiser: Not at all. In the beginning, the first few days after an infusion, I was sleepy and tired. That may have impacted it a tiny bit, but nothing significant. For the past six to nine months, it hasn’t bothered me at all.
Being Patient: So physically, since your diagnosis, you’ve been able to keep up the same pace as your training?
Scott Berkheiser: Yes, exactly.
Being Patient: And what about your training? What do you have coming up in those races? Are you still going to compete?
Scott Berkheiser: Yes. The interesting thing about an IRONMAN or even marathons, [is that] you have the pros, you have the age groupers that are competing as amateurs, and then you have people whose goal is just to beat their time or finish. That’s the category I fall into. I don’t have the body and build to be able to go the speeds the serious competitive athletes do in triathlon. It’s mind-boggling what they do on the bike and the run and the swim. It’s a matter of endurance. I’m racing myself. The goal is to finish.
Being Patient: Are you involved with Alzheimer’s groups? Do you represent them in the races?
Scott Berkheiser: Yes. I got hooked up with the Alzheimer’s Association by a gentleman named Dan Jaworski. When I got diagnosed, probably within the first couple of days after diagnosis, I googled IRONMAN and Alzheimer’s, and Dan Jaworski’s name popped up. So I reached out to him. It was great, especially at that time, early-onset was still not that recognized. He basically [directed me] to the Alzheimer’s Association.
“I’m racing myself.
The goal is to finish.”
A week or two went by and I got a phone call. The next thing I knew, I was giving speeches and going here and going there. It made me feel good that [I] could talk to people because it’s a topic that people don’t really like to talk about. It’s kind of one of those things that a lot of people stay quiet about. To be able to actually speak publicly, go to see our senators and congressmen and do all those things, it kind of gives me a purpose.
Being Patient: Do you find an extra purpose when you’re running now? To almost represent a community too?
Scott Berkheiser: I do. My last full IRONMAN in Texas, the wind was absolutely brutal. It was sustained at 35 [mph], gusting to 42 [mph]. It was miserable. There was a point where I stopped at a rest aid station and there were a bunch of people a lot younger than me that were just giving up. They were waiting for the van to come pick them up. I’m sitting there going, “These guys are 20 years younger than me and they’re going to give up. How am I going to finish?” Then, I kind of remembered back to what got me through life. My dad [would say], “Don’t give up, as long as you try your best it’s all that matters.”
So I just got on my bike and started pedaling. I’m thinking about it and I’m thinking about all the people with the Alzheimer’s Association that have raised money and all the awareness they’ve done and all the publicity. And I’m like, “Well this is going to look really bad if I don’t finish the race.” That gave me the motivation to just keep pushing on and get through it and finish it.
Being Patient: Do you hear those words just in your daily life from your father, too, about persevering when you may get frustrated and not remembering things?
Scott Berkheiser: Yeah, I do. I think our brains were sort of similar. I know he would have been frustrated himself, but always give your best, whatever else happens doesn’t matter — that’s how I’ve lived my life.
Being Patient: And you worked in the aviation industry, too. Tell me about that and how that was impacted by your diagnosis?
Scott Berkheiser: I spent most of my career working on stealth aircraft, stealth technologies. The military has a stealth version of everything — rifles, soldiers’ helmets, anything you don’t want a radar to be able to pick up. I was involved in the equipment and test facilities that actually test the airplane, the missile, the ship, whatever, to make sure the stealth technology is doing its job effectively and nobody gets a surprise.
Being Patient: When you got the diagnosis, did you continue working?
Scott Berkheiser: I worked another year and a half.
Kris Berkheiser: He just retired this year.
Being Patient: Another interesting tidbit from your life is that you started out this whole sort of adventurous spirit by getting into go-kart racing, and that got you into IRONMAN racing, is that right?
Scott Berkheiser: Yes, it did. I think I was bored when I stopped racing and had to do something. I started running just to get in shape. I was running around the neighborhood and I saw a sign for a half marathon coming up in Hilton Head in six months. And I’m like, “I can run five miles, maybe I can do that.” That was what started me down that path. My first race was a half marathon and then I did a full, and then that’s when I kind of switched over into the triathlons and then worked my way up to the IRONMAN races.
Being Patient: Kris, how are you involved in this adventurous lifestyle that Scott has to live constantly, and now with the challenge of Alzheimer’s? Are you providing some extra care in the training to make sure that everything’s going right?
Kris Berkheiser: Well, I’ve always been his support crew. What he does is, in my eyes, impossible. I don’t know how he does it. But the only thing that I’d say that I help additionally with now is just making sure he doesn’t stress over things that he thinks he’s forgetting. Because sometimes he thinks he’s forgetting things when he’s not. Stress is probably his biggest enemy. Honestly, the training is very therapeutic for him. He’s much happier if he’s training every single day. He actually is a little anxious on the one day a week that he doesn’t train. I don’t provide much other than just support.
“What he does is, in my eyes, impossible.
I don’t know how he does it.”
Scott Berkheiser: Her job starts after the race is over because in an IRONMAN , when you stop, your body finally shuts down and everything starts cramping. She helps get me through that part of it — feeding me and giving me fluids. When something cramps, she’s working the cramp out.
“If you suspect you have Alzheimer’s or some
form of dementia, don’t wait. Especially if
you’re younger, doctors tend to push it off.
Get checked out, go to a neurologist, get second opinions.”
Being Patient: Any final words that you can offer to our audience?
Scott Berkheiser: If you suspect you have Alzheimer’s or some form of dementia, don’t wait. Especially if you’re younger, doctors tend to push it off. Get checked out, go to a neurologist, get second opinions, because we now, for the first time, have a treatment that actually slows the disease. It’s not a cure, but it slows the disease. The way I look at it, if I get an extra 12 months, 18 months, two years — what’s the price tag on that? It’s priceless. The sooner you get started, the better.