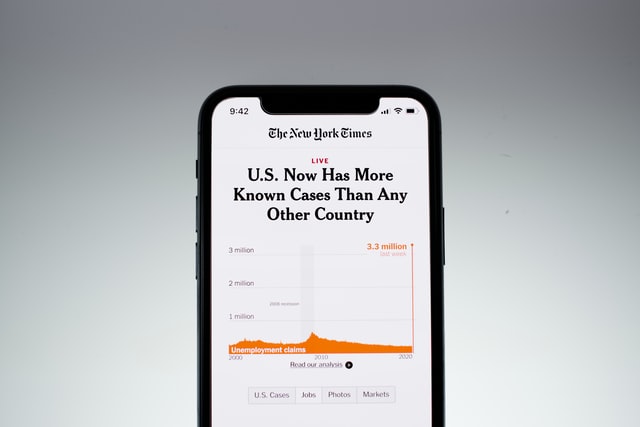
The public health repercussions of contracting COVID-19 have been front-and-center for months. Beyond the disease’s physical effects, researchers say that its psychological toll may also be far-reaching.
Clinicians have found that COVID-19 patients with mild physical symptoms may experience psychological distress in the short term, including anxiety and depressive moods. Researchers now wonder whether people who are infected will suffer from the long-term psychological consequences as well.
Short-term Anxiety and Depression Linked to COVID-19 Patients’ Loss of Smell
In a recent study, researchers surveyed 114 patients diagnosed with COVID-19 over a six-week period. About 47 percent of participants reported experiencing a depressed mood for at least several days of the week, and about 20 percent felt depressed almost every day. And nearly 56 percent of participants reported experiencing mild to severe anxiety.
“There’s a very high prevalence of depressed mood and anxiety in these patients,” said Ahmad Sedaghat, an author of the study and an associate professor and director of rhinology, allergy and anterior skull base surgery at the University of Cincinnati. “So far, it’s unquantified and under-appreciated. That’s something we need to keep in the back of our minds when we treat these patients.”
Infections of SARS-CoV-2 typically begin in the nose and mouth, which can then spread to the lungs. And Sedaghat’s past research shows that people who suffer from conditions of the upper airway, may experience significant psychological burden. For instance, patients with chronic rhinosinusitis are at a higher risk for depression. The inflammatory disease occurs when sinuses become swollen and inflamed for a period of time. People can also experience symptoms such as nasal blockage and a loss of smell and taste.
Those who are infected with SARS-CoV-2 can also lose their sense of smell or taste. According to Sedaghat, people may feel anxious when their sense of smell falters, as they lose the ability to pick up on the odor of their bodies, detect whether there have been chemical leaks at their homes, or sense the aroma of their food.
But the team found no association between patients’ more severe symptoms – cough, fever and shortness of breath – and how anxious or depressed they felt, a finding which Sedaghat found shocking: “You would think that the symptoms which are predictive of the most dire outcome would be the symptoms associated with anxiety and depressed mood. That really wasn’t the case.”
On the other hand, the only predictors of how depressed and anxious patients felt were the the severity patients’ loss of smell or taste, which may indicate another factor contributing to people’s psychological symptoms.
“No one is going to die from olfactory dysfunction … Yet somehow, it was most associated with depressed mood and anxiety,” Sedaghat said. “This really got us thinking about why this could be the case.”
“It is very possible that this association is actually indicating that central nervous system penetration of the virus could be driving this psychological distress that we’re detecting,” he continued.
Sedaghat suggested the virus may attack the central nervous system by entering the olfactory tract, a bundle of nerve fibers connected to a system that regulates smell and taste.
Past studies provide clues of the virus’ ability to penetrate the central nervous system. There is evidence that its relative, SARS-CoV-1, can infect the brain via the olfactory system.
And studies have also shown that COVID-19 patients can suffer from central nervous system complications like altered mental status and stroke. These are rare symptoms, Sedaghat noted, but depressed mood and anxiety could very well be the more common signs of the virus penetrating the central nervous system.
“It’s just that we haven’t been thinking about psychological distress as a central nervous system manifestation of the disease, which is why we really haven’t found this association before,” he said.
More research is needed to pinpoint whether or not SARS-CoV-2 can directly invade the brain. Though what’s clear from the study is that people infected with the novel coronavirus are bearing the emotional tolls of an infection even when they experience mild symptoms such as the loss of smell and taste.
And the researchers wondered whether these short-term psychological symptoms would lead to more persistent mental health problems: “This is a significant burden and has a significant negative impact on the quality of life,” Sedaghat said. “These poor patients have gone through this terrible disease. They’ve recovered. But now, are they going to have long-term effects of psychological distress?”
Potential Long-Term Consequences of Neurological Symptoms
Other researchers have also raised the question of whether COVID-19 may lead to long-term mental health conditions amid growing evidence detailing the neurological complications among COVID-19 patients such as delirium and brain damage. Clinicians worry that neurological disorders may increase people’s risk for mental health disorders, warning of a wave of patients in the coming years with conditions such as depression and anxiety.
Past research on SARS-CoV-1, the virus that caused the 2003 SARS outbreak, shows that many survivors suffered from persistent mental health problems and chronic fatigue 31 to 51 months after the epidemic. More than 40 percent of them suffered from psychiatric illnesses like post-traumatic stress disorder, depression and obsessive-compulsive disorder.
Though researchers say it’s too early to tell if COVID-19 can lead to lifelong neuropsychiatric disorders. In the meantime, they are urging clinicians and patients alike to be vigilant for the neurological and psychiatric complications of infected patients.
“[Patients] may have a little problem sleeping, their mood might be a little off, maybe they are a little bit depressed,” Majid Fotuhi, a Johns Hopkins University affiliate staff member, said of infected patients who may experience mini strokes. “But they would not think that these symptoms are due to SARS-CoV-2 infection. They would just go on with life.”
The Psychological Toll Extends Beyond Patients to Their Loved Ones
As COVID-19 cases and death rates continue to rise, the number of families bearing the emotional burden of losing loved ones during the pandemic are growing. More than 1.3 million American families have lost a close family member due to COVID-19 as of Monday, according to a tracker created by researchers in a recent study. Among them are more than half a million Americans who have lost a grandparent from the disease.
“We are going to see the ramifications of the bereavement of this pandemic for years, if not decades to come,” said Naomi Saks, a clinical health care chaplain and associate director of the inpatient palliative care service at University California of San Francisco Medical Center, who was not involved in the study.
Saks recounted a man’s father who contracted COVID-19 and passed away. After the family attended the funeral, another four of his family members were infected. While one of the man’s daughters survived, the rest of the infected family members died. “Each life loss is a person. It’s a story, a family affected,” said Emily Smith-Greenaway, an author of the study and an associate professor of sociology and spatial sciences at University of Southern California.
“Wear a mask, stay at home [and] physically distance from others when you can,” Smith-Greenaway said. “It’s not only saving your family from unnecessary grief, but it’s also potentially saving others in your community from trauma, grief and losses, which are avoidable.”
Researchers warned about another wave of public health challenges as families are beset by the loss of loved ones, grieving during a time of COVID-19 restrictions when physical contact and travel are limited.
Restrictions for funerals and memorials have also disrupted how families grieve due to the pandemic, a shared reality for families mourning for loved ones who died of the coronavirus and other medical illnesses.
There are still ways to honor the memories of a loved one during the public health crisis. It’s not the same, admitted psychologist Dale Atkins, who was not involved in the study, but they do help families find some sense of closure. She pointed to a friend who held a Zoom funeral after losing her mother to a medical illness in mid-march. She saw loved ones who lived far away, friends and family who would otherwise have been unable to attend the funeral.
People were invited to speak and one woman sang her mother’s favorite song. Her friend was so moved and engaged, Atkins said, touched in a way that helped her find closure.
“You can be creative in nurturing yourself and honoring the memory of the person while being able to recognize the profundity of the loss,” Atkins said. “And we’ll get through.”
Meanwhile, the daughter of the family that had suffered the loss of four family members from COVID-19, Saks said, recovered and looked forward spending time with her family upon discharge.
“The family found a strength inside themselves that they never knew was there,” Saks said. “[The pandemic] has hit all of us hard. It has broken our hearts … but it hasn’t taken away the love of families, stories and the courage of the caregivers and the patients. It hasn’t taken away the human spirit — the essential human spirit that wants to live and thrive and adjust to change.”