The FDA approved a new dosing regimen for Lilly’s Alzheimer’s drug Kisunla intended to reduce the risk of side effects and make the drug safer.
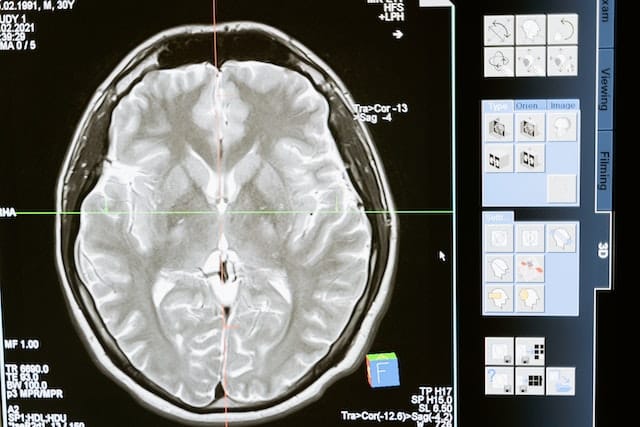
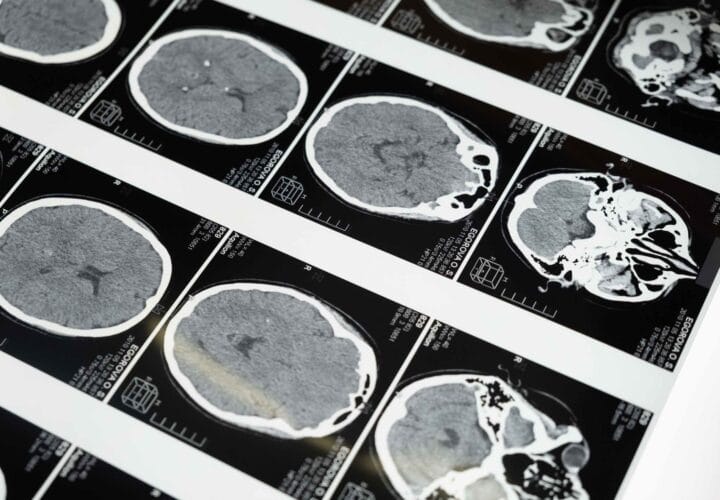
In July 2024, the Food and Drug Administration approved Eli Lilly’s anti-amyloid drug Kisunla for people in the earliest stages of Alzheimer’s disease. It’s part of a new class of monoclonal antibody drugs for Alzheimer’s that don’t just treat the symptoms — they’re designed to actually modify the disease itself, by clearly plaque build-up out of the brain. Taking this approach, the drug does appear to be effective in slowing in disease progression, at least slightly. And that slight improvement comes at a cost: Some patients develop the side effect of brain swelling and bleeding (ARIA), and at a higher rate than Kisunla’s anti-amyloid competitor, Leqembi.
The drug’s side effect profile contributed to the decision by European regulators to reject the drug’s approval earlier this year. But due to a newly FDA-approved dosing regimen where patients take less of the drug over a longer period of time, regulators and the drugmaker hope treatment with Kisunla will now be safer.
The new dosing regimen was validated in a clinical trial called TRAILBLAZER-6, which found that a more gradual increase in dosing would reduce the risk of ARIA, which is most common early in treatment. ARIA is often mild or asymptomatic, but in rare cases, it could be life-threatening. Many patients who develop ARIA stop treatment and then resume once it resolves.
The original dosing regimen involved providing patients with two vials of the drug for the first three infusions, then increasing to four vials. The new dosing regimen involves one vial during the first infusion, two vials during the second, and three vials for the third infusion before increasing to four vials.
By week 24, almost one quarter of patients on the regular dosage developed brain swelling compared to 14 percent with the new dosage. After a year, a quarter of participants at the regular dose had developed brain swelling compared to 16 percent on the new dosage.
This new, more gradual dosing increase didn’t seem to affect the drug’s plaque-clearing abilities. (While Europe had rejected the drug outright, Australian regulators have already approved Kisunla with this lower dosing regimen.)
“This updated dosing strategy is a meaningful advancement for patients and their care teams,” Dr. Elly Lee, MD, chief medical officer at the Irvine Center for Clinical Research, said in a press release.
After the data were presented at an Alzheimer’s conference last year, Dr. Suzanne Schindler, a neurologist and researcher at Washington University School of Medicine in St. Louis, said their clinic planned to institute the new dose regimen for Kisunla. “I really see no disadvantage of doing this, and if it makes treatment with these therapies safer, that it’s an obvious thing to do,” she told Being Patient.
Since the new dosing regimen still uses the same number of vials to treat patients, it won’t bring the cost down. The total cost depends on how long someone needs to take the drug to clear out their plaques. The estimated minimum cost is $12,522 for six months. It could peak at $48,896 for a year and a half. For most patients, this expense is covered by Medicare.



Interesting information! I have had 3 infusion and after 3 mri no change!
Interesting information! I have had 3 infusion and after 3 mri no change!