Scientists identified new genes that impact the brain’s immune cells and may contribute to the risk of developing early-onset or late-onset Alzheimer’s.
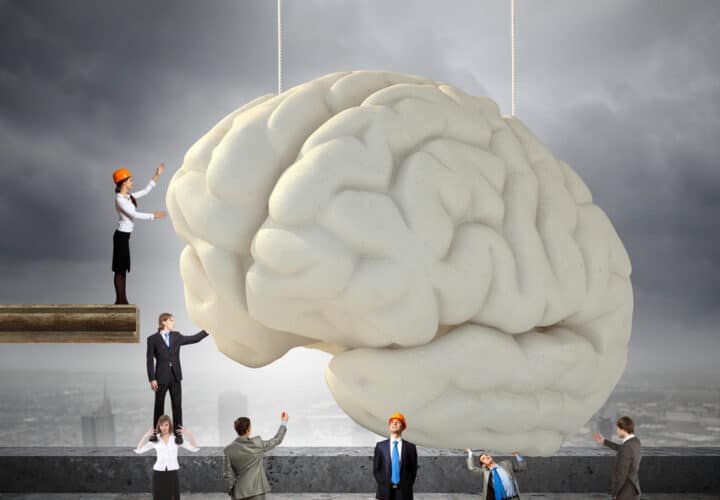
The brain’s immune cells, known as microglia, are located in the brain and spinal cord. They serve as the main immune defense in the central nervous system. They also work as the brain’s cleaning cells, removing plaques and damaged neurons.
The Brain’s Cleaning Immune Cells
In the study, researchers pinpointed two genes found in the microglia, MS4A4A and TREM2. These two genes were found to influence the levels of a protein also known as TREM2. Scientists believe the TREM2 protein is responsible for boosting the microglia’s ability to clear out amyloid and tau — the toxic proteins involved in Alzheimer’s disease — from the brain.
When the two identified genes alter levels of the TREM2 protein, it may worsen the risk for developing Alzheimer’s disease, because the proteins don’t have the chance to clear out tau and amyloid.
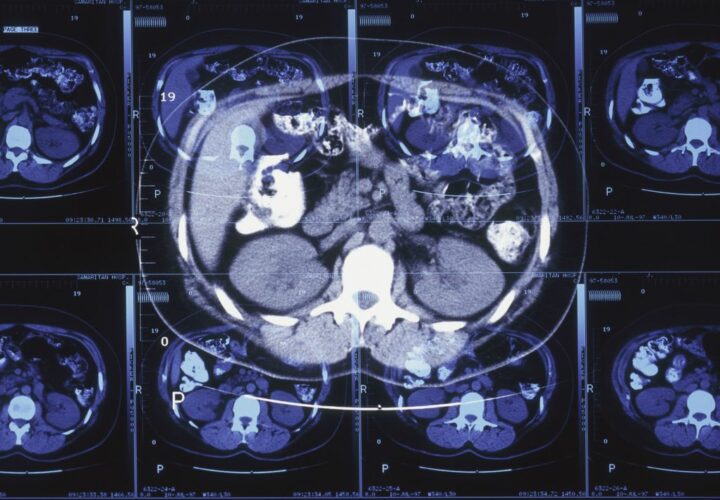
The study examined 813 older adults. Some of the participants had Alzheimer’s disease, some were considered cognitively normal and some had mild cognitive impairment.
“We observed TREM2 risk variants more often in people who had Alzheimer’s or were mildly cognitively impaired, compared with those who were cognitively normal,” said Celeste Karch, assistant professor in the Department of Psychiatry at Washington University School of Medicine in St. Louis, in the press release.
Karch noted that about 30 percent of the population in the study showed some level of variation with the MS4A4A gene, which could either increase their risk of developing Alzheimer’s disease. In some cases, it could protect them from it.
“Some variants protected people from Alzheimer’s or made them more resilient while others increased their risk,” Karch said.
Microglia’s Potential in Alzheimer’s Therapies
Researchers have been delving into how genes impact Alzheimer’s disease for some time now, including the ApoE4 gene, to help develop new genetic therapies.
The latest study’s focus on the MS4A4A and TREM2 genes hint at a new way of looking at a potential intervention for the disease. Instead of focusing solely on neurons, the researchers emphasized the value in studying the microglia’s role in clearing bad proteins like beta-amyloid and tau.
“The findings point to a new therapeutic strategy,” Carlos Cruchaga, professor of psychiatry and director of the NeuroGenomics and Informatics Group, said in the press release. “If we can do something to raise levels of the TREM2 protein in the cerebrospinal fluid, we may be able to protect against Alzheimer’s disease or slow its development.”
The brain’s immune cells may even play a role in other neurodegenerative and inflammatory diseases, making them interesting subjects for further study.