There is no single test available to diagnose Alzheimer’s. Instead, physicians rely on several diagnostic tools and medical criteria to ascertain whether a person may be suffering from the disease. Unfortunately, the most widely recognized diagnostic tests for Alzheimer’s are inconclusive, at best. And while neurologists and geriatricians can usually tell if a patient is suffering from dementia, figuring out its cause is challenging, and may lead to a false Alzheimer’s diagnosis.
Why an Alzheimer’s Test and Early Diagnosis Is Important
Last year, an ongoing study found that one-third of patients diagnosed with Alzheimer’s didn’t have beta-amyloid plaques—a protein that accumulates in Alzheimer’s and is considered a biomarker of the disease. A mistaken diagnosis can lead not only to unnecessary emotional trauma, but also cause a patient to lose valuable time if they actually have a treatable disease that isn’t Alzheimer’s.
“Failing to detect dementia can delay access to treatment and support, whereas false alarms lead to unnecessary investigations, causing pressure on health care systems,” said Llewellyn. “Identifying people with dementia in a timely fashion is important, particularly as new methods of treatment come on stream. Our findings show that we desperately need more accurate and less biased ways of detecting dementia swiftly in clinic,” says author David Llewellyn, Ph.D., of the University of Exeter Medical School in the United Kingdom.
An early and accurate Alzheimer’s diagnosis gives patients and caregivers a chance to plan out their care and quality of life decisions. It also gives them the opportunity to use medication that helps control symptoms in the early stages of Alzheimer’s.
Alzheimer’s Tests – What to Expect During an Exam
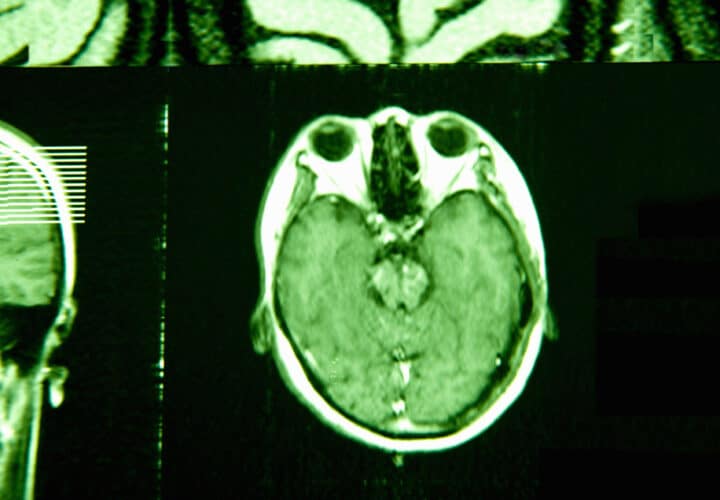
The only definitive Alzheimer’s test that exists right now is a post-mortem examination of the brain in a lab. This tells physicians whether the patient had tau tangles and beta-amyloid plaques in his or her brain.
Still, physicians do have other methods of assessing memory problems and landing on an Alzheimer’s diagnosis.
Related: New Alzheimer’s Test More Accurately Predicts Risk Than ApoE4 Gene
Medical History and Physical Exams to Rule Out Other Conditions
Before performing any Alzheimer’s tests, your doctor will carry out a medical exam and go over your health history, including history of emotional health issues, and cognitive and behavioral changes. Your health provider will want to know what conditions run in your family, what medications you’re taking, and about any past illnesses.
Alzheimer’s and other types of dementia have many of the same symptoms as other health conditions, such as depression, medication side effects, insomnia or untreated sleep apnea, vitamin deficiencies and excessive alcohol consumption.
Neurological Exams to Test for Alzheimer’s
These tests, which involve examining speech, sensation, eye movement, coordination and strength, and reflexes will evaluate whether the person might have other brain disorders, such as brain tumors, a stroke, Parkinson’s disease, and other conditions that may affect memory.
Memory Status Tests for Alzheimer’s: The Pros and Cons
Memory tests, like the Mini-Cog and Mini-Mental State Exam (MMSE), are commonly used to assess one’s risk of Alzheimer’s.
Many are available to download online and may ask patients to recall an unrelated string of words, such as: banana, sunrise and chair, or ask the day of the week. These tests, which take just minutes to administer, can deliver the troubling news of a dementia diagnosis and are used in clinical trials to measure cognition. But a new study has found that quick memory tests like these are giving misleading results across the board.
The study, printed in the journal Neurology Clinical Practice, a publication of the American Academy of Neurology, looked at three studies: the Memory Impairment Screen, a test that measures word recall; the Mini-Mental State Examination, which asks questions like “What day is it?” and also measures the ability to remember words; and Animal Naming, a test asks patients to name as many animals as possible in one minute.
They found that the tests were often inaccurate, delivering a diagnosis that wasn’t always right.
“Our study found that all three tests often give incorrect results that may wrongly conclude that a person does or does not have dementia,” said the study’s author David Llewellyn, Ph.D. “Each test has a different pattern of biases, so people are more likely to be misclassified by one test than another depending on factors such as their age, education and ethnicity.”
Much like standardized tests children take in schools, which have shown a cultural bias rooted in social class, race and region, dementia tests were found to have a bias related to race, education level, age and living situation.
To carry out the study, researchers gave all three tests to 824 people in the U.S. with an average age of 82. But first, they diagnosed them with dementia based on a physical exam, genetic testing for the ApoE gene, a gene which most accurately determines Alzheimer’s risk, and psychological testing, along with more extensive memory and thinking tests. Based on those tests, they determined that 35 percent had dementia and 65 percent did not.
Related: What You Should Know Before Getting a Genetic Test for Alzheimer’s
When they then gave them the three quick tests, they found that 36 percent of participants were wrongly classified—including false positives and false negatives—by at least one of the tests. Two percent were misclassified by all three tests. On an individual test basis, 4 to 21 percent were misclassified.
Meaning, don’t take one test as gospel. If you’re going to take a memory test for Alzheimer’s, be sure you take all three.
Scientists found that depending on the test and the patients background, some tests were easier than others—even for those with dementia. One test was found to have an education bias, showing that people who were more educated could compensate for their thinking problems with a cognitive reserve. Those who did have dementia with a higher education were more likely to be mistake as not having dementia, while those with less education were more likely to be mistaken for having it. Being a race other than white also led to more false diagnoses, along with being older or living in a nursing home. All of the tests showed that a lack of input from loved ones increased the risk of mistaken diagnosis.
The findings align with advice from leading experts. As Dr. Bill Burke, of the Banner Alzheimer’s Institute, told Being Patient founder Deborah Kan, the best person to ask about your memory is the people closest to you.
“You could do elaborate neuropsychological testing and none of it is as effective as asking the person who really knows [you],” said Burke.
Read Next: Is There an Alzheimer’s Blood Test?



Believe our pcp uses the mini-cog, which my husband very proudly aces! I drive him to his appointments because he can no longer remember how to get there. I know he had some sort of dementia, but with no doctor’s diagnosis, he isn’t eligible for any of the meds for early-stage dementia. Four appointments and four “you’re just fine” from our doctor – I think he thinks I’m the one with a problem! Husband is in total denial so I can’t do much. Any suggestions?
If possible, get a second opinion from a neurologist who specializes in cognitive issues. Good luck.
Where are the references? Hard to take this seriously…
My Optometrist says there is an eye test that shows if one has ALZ and offered it to me, I said no, what would I do with the information? When there’s a cure I’ll take the test. My Mother passed from ALZ>
I need the truth. I can live with the consequences, and hope for future help with the treating the disease.