How often do damaged blood vessels occur in concussions — and could affect the way head injuries should be treated?
What’s happening inside the brain during and after a traumatic brain injury is still an active area of research. While nerve damage from hits to the head is considered a major factor in concussions, one 2019 study aimed to examine whether there were other factors at play. The researchers focused on the extent to which damaged blood vessels occur in concussions, and whether this could impact the direction of future therapies.
Traumatic brain injuries (TBIs) are caused by blunt hits to the head, whether due to a fall, accident or injury from a contact sport. Some of the physical symptoms of a TBI can include loss of consciousness, headache, vomiting, fatigue or dizziness. It’s also possible to experience blurred vision, ringing in the ears or mental health problems as a result of a TBI—including mood changes or depression.
The long-lasting effects of traumatic brain injuries are still being investigated, but some research has shown that these hits to the head can increase the risk of developing neurodegenerative diseases. It’s possible that TBIs may trigger inflammation in the brain and lead to dementia. Consistent concussions or sub-concussive hits over the long-term can also result in the development of chronic traumatic encephalopathy, or CTE, a brain disease defined by behavioral, mood and thinking problems.
Blood Vessel Damage
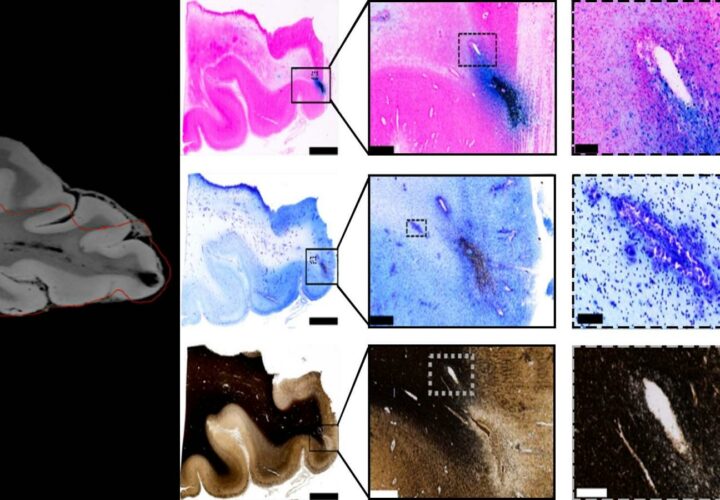
In the study, the researchers took scans of a deceased person’s brain with a high-throughput neurohistological pipeline, a method for visualizing brain slices that allowed for higher-quality images.
They also used MRI scans to identify where the head trauma had left physical imprints on the brain, lesions they refer to as “black blobs.” In order to differentiate between nerve and blood vessel damage, they used an iron stain to make blood stand out as blue, and a myelin stain to make nerve fiber fragments pop out.
Blue-stained blood cells appeared where the lesions were, the researchers found, which meant that blood vessel damage and traumatic microbleeds occurred in those areas. At the same time, there wasn’t as much of an indication that nerve damage had also happened based on the myelin stains.
The researchers concluded that there were more signs of blood vessel damage than nerve damage.
“Nerve damage following traumatic brain injuries has been a majority point of view, and therapy as well as drug development has been targeted towards that,” Partha Mitra, Cold Spring Harbor Laboratory professor and an author of the study, said in a news release. “The idea is that if the mechanism is actually different, therapeutic intervention may also be different.”
Ultimately, “recognizing traumatic microbleeds as a form of traumatic vascular injury may aid in identifying patients who could benefit from new therapies targeting the injured vasculature,” the researchers wrote.
Image: Tissue imaging confirms blood vessel damage in traumatic brain injury patients. Courtesy of Mitra lab/CSHL, 2019.