When a researcher’s spiders began showing signs of brain degeneration, she discovered a new waste clearance pathway in their brains that could have implications for Alzheimer’s in humans.
Fruit flies. Zebrafish. See-through worms. All critters you’d expect to see in an exotic pet store or in an Amazonian lagoon. But small, strange organisms like these are also ideal for helping scientists better understand the inner workings of humans’ brains.
One such model organism — the Central American wandering spider — is perfect for this, because its brain cells are very large relative to their body, making them easier to study. So when Ruth Fabian-Fine, professor of biology and neuroscience at Saint Michael’s College in Vermont, noticed that these spiders couldn’t crawl up walls or hunt prey efficiently, she decided to investigate. “They all showed neurodegeneration at young ages,” Fabian-Fine told Being Patient.
What she discovered was that a pathway in their brains — usually meant to clear waste — was going haywire and making the spiders behave oddly. The findings from her research, conducted with NIH grant funding and published in the Journal of Comparative Neurology last year, suggest a link between the phenomenon in the spiders’ brains and Alzheimer’s in humans.
What happened to the spiders?
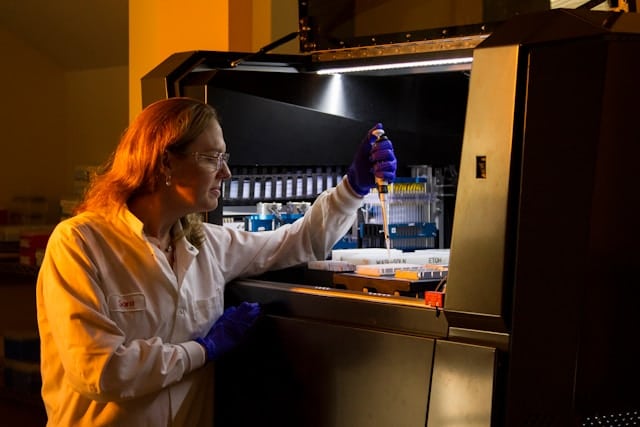
Fabian-Fine and her colleagues dissected the spider’s brains and used microscopes to look for clues. The supportive cells of the brain, the astrocytes — which are involved in waste clearance, signaling, and mounting an immune response — had sprouted canals that connected to neurons.
While these strange structures weren’t previously characterized by other scientists, they were familiar to Fabian-Fine, who first spotted the canals in graduate school.
She believes they work like vacuums. A protein called aquaporin-4 lined their walls, which allowed liquid waste from neurons to be sucked up by the astrocytes. In the spiders that developed neurodegeneration, the tunnels were bloated and overflowing with waste.
Fabian-Fine hypothesized that the canals were sucking up too much, depleting the cells of their contents, causing them to degenerate and die.
What caused these tunnels to fail in the first place? The protein machinery that held the canals together was temperature-sensitive. Too cold, and they can’t work properly. “The window that the spiders were on had a draft in the wintertime,” said Fabian-Fine. “That’s why these canals unraveled and brought these neurons to neurodegeneration.”
Do humans also have this waste clearance system?
Many important discoveries that impact human health start off as curious observations in other organisms.
“By studying the nervous systems of other organisms, we gain valuable insights into potential functions of our own cells that can ultimately lead to a much better understanding of disease,” Melissa Cooper, a scientist at NYU Langone who wasn’t involved in the research, told Being Patient.
Working with a neuropathologist, Fabian-Fine spotted cells with nearly identical features in the memory region of the brain, called the hippocampus, in postmortem brains.
These astrocyte cells, called ependymal glia, were found near the brain’s ventricles. That’s significant: Ventricles are cavities within the brain that carry cerebrospinal fluid and may help the brain eliminate waste. Fabian-Fine thinks these canals might be trafficking waste out of the brain through the ventricles in healthy people.
But in the brains of people who died with Alzheimer’s disease, these canals also looked swollen. The nearby neurons were “empty”, almost as if the canals had sucked out all their contents. The researchers also found the hallmark proteins of Alzheimer’s disease, beta-amyloid and tau, near these canals too.
Cooper said the study “could have broader implications on our understanding of the clearance of problematic proteins, such as amyloid.” The connection between the brain’s waste clearance pathways and brain health has been a hot topic of debate among neuroscientists — some believe it to be a missing piece of the Alzheimer’s puzzle while others question its role.
Fabian-Fine also thinks that microbes might cause trouble for these canals, potentially sparking Alzheimer’s. In the last few years, more evidence emerged linking Shingles, Herpes, and other infections to Alzheimer’s, as well as some evidence that preventing or treating infections could reduce risk.
“Alzheimer’s patients have a very high incidence of fungal, bacterial and viral infections,” said Fabian-Fine. “If you have a canal system, you need to break down this debris, because if you don’t break it down, there’s the danger of blocking this canal system.”
Her research group is now looking at a fungal protein called chitin to see if it’s messing with the vacuum.
The research was supported in part by an NIH grant (P20GM103449).