Mounting evidence shows that Alzheimer's biomarker tau protein accumulates differently — and more rapidly — in woman's brains than in men's.
Over 30 million people live with Alzheimer’s disease worldwide, making it the most common form of dementia. Two thirds of those diagnoses are women. Scientists used to attribute this discrepancy to the fact that women on average live longer than men. But recent studies have linked Alzheimer’s to menopause, hormones like estrogen, number of pregnancies, lifespan of fertility. One study even found that after age 45, about half of women will experience either a stroke, or the onset of Parkinson’s or dementia, compared to about one third of men. Yet, research has also shown that women’s brains age more slowly than men’s. So, why is their Alzheimer’s risk higher?
Mounting evidence suggests that a distinction in the chemistry or structure of women’s brains may be a factor — a distinction that may lead to a sex-based difference in the appearance and aggregation of tau and beta-amyloid proteins, key biomarkers of Alzheimer’s. In a 2021 study published in Brain, researchers at Lund University in Sweden found evidence that the protein tau accumulates at a higher rate in women.
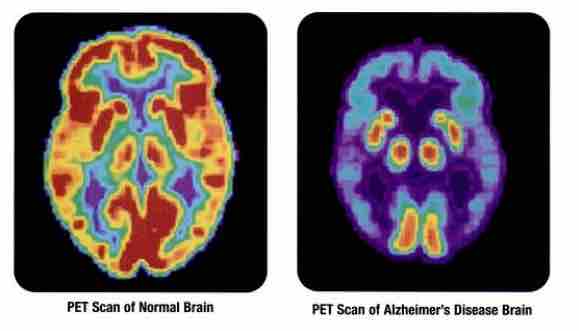
The toxic proteins behind Alzheimer’s disease
In the first stages of the disease, the team found that among a cohort of 209 women and 210 men, both sexes were equally affected, with no apparent differences in the accumulation of beta-amyloid. Later, when tau proteins starts to clump in the brain, memory dysfunction sets in. After adjusting for age and the levels of tau they had at the beginning, the researchers found that at this point, more women than men appeared to have Alzheimer’s-related memory problems — and, they had higher accumulations of tau.
“Tau accumulation rates vary greatly between individuals of the same sex, but in the temporal lobe, which is affected in Alzheimer’s disease, we found a 75-percent higher accumulation rate in women as a group compared to men,” Ruben Smith, first author of the study and a professor at Lund University, said at the publication of the study.
Why are women more likely to develop Alzheimer’s?
The team says the next step is to examine why this accumulation is faster in women.
“Our study strongly indicates that the faster spread of tau makes women more prone to develop dementia because of Alzheimer’s pathology compared to men,” added Oskar Hansson, an author on the study and a professor at Lund University. “Future experimental studies will be important to understand the reasons behind this.”
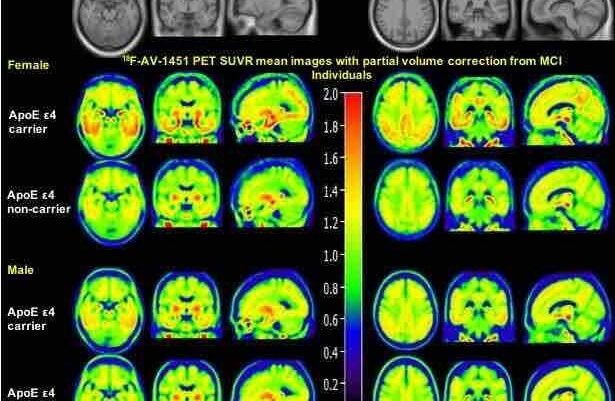
Previous research from Vanderbilt University might hold a clue: In 2019, a team looked at the PET scans of healthy people and patients with mild cognitive impairment — often a precursor to Alzheimer’s — and found that the structure of tau networks is different in men and women; women had more “bridging regions” connecting different regions of the brain. The researchers theorized this difference may be what allows tau to spread more easily across the brain, accelerating the development of Alzheimer’s.
These are yet still just theories — to confirm it, more research is in order, and some women’s health advocacy groups are calling on the research community to adjust their approach.
Considering male vs. female as a biological variable in Alzheimer’s research
The Society for Women’s Health Research (SWHR) is advocating for better incorporation of sex as a biological variable (SABV) into Alzheimer’s preclinical research, from incorporating more female mice into studies to creating a “best practices” approach for incorporating SABV, updating minimum inclusion standards and never failing to consider data from a SABV-based perspective.
“For decades, researchers have largely ignored sex as a biological variable within preclinical studies,” authors from SWHR wrote in an editorial recently published in Alzheimer’s & Dementia: Translational Research & Clinical Interventions. “Recent literature indicates scientists are increasingly including male and female subjects in studies, but fewer studies assess for sex differences in study outcome. This is particularly concerning within the field of Alzheimer’s disease, as disease burden is higher among women and evidence suggests sex differences exist in etiology and disease course.”
Meanwhile in an op-ed for Being Patient, Carolee Lee of WHAM! (Women’s Health Access Matters) and Michelle M. Mielke at the Specialized Center for Research Excellence on Sex Differences at Mayo Clinic examine the consequences of ignoring gender and biology in Alzheimer’s research — and the pivotal importance of lifespan research.
“Investing in research that looks across a woman’s lifespan to identify risk factors for Alzheimer’s disease and related dementias can help women monitor early warning signs and potentially mitigate risk factors that can prevent or delay the onset of cognitive impairment,” the authors wrote. “This research has the potential to save millions of lives that would otherwise be lost to Alzheimer’s, and to significantly reduce the hefty price tag that Alzheimer’s disease and related dementias presents for patients, families, caregivers and our healthcare system.”
Lowering Alzheimer’s risk, boosting brain health
So what can women do to keep their brain in check? Dr. Marie Pasinski, a faculty member at Harvard Medical School and neurologist at Massachusetts General’s Institute for Brain Health, told Being Patient that women should focus on the things they can control that lead to better brain health.
“One of the most important things is staying on top of your physical health,” Pasinski said. Recent studies have looked at modifiable risk factors, including underlying medical issues like midlife obesity, hypertension, diabetes, smoking, depression and insomnia. Some research indicates that addressing these factors can prevent up to 40 percent of dementia cases.
“If you have any of those underlying conditions, make sure you’re getting the best treatment you can get and all of those medical problems under control,” Pasinski said. “That will significantly decrease your risk of Alzheimer’s.”
UPDATE 13 April 2023: This March 2021 article has been updated with new information to help our readers.



Some fundamental differences in the structure of the tau protein for males and females should be observable in DNA type analyses, and related to the hormonal chemistry. Then, CRISPR gene editing could be more effective in alleviating symptoms. Also, is there a difference in EEG measuements of brain wave spikes for men and women that could be alleviated by a drug line levetiracetam?