Carolee Lee of WHAM! and Michelle M. Mielke at the Mayo Clinic examine the consequences of ignoring gender and biology in Alzheimer’s research — and the pivotal importance of broad lifespan research.
Photo: Carolee Lee, left and Michelle M. Mielke, right; Courtesy of Women’s Health Access Matters!
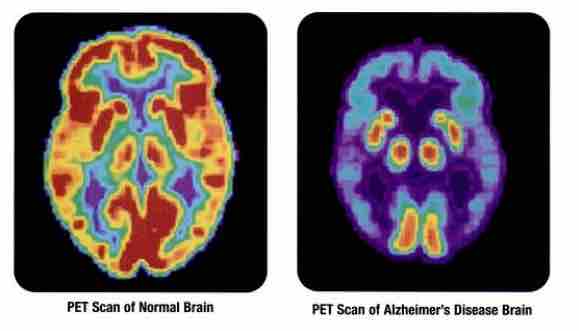
Alzheimer’s disproportionately impacts women, who make up two thirds of the 5.7 million Americans living with the disease. Beyond the raw numbers of those affected are significant differences in disease progression, outcomes, and hundreds of new questions for researchers and clinicians to explore. Today the economic consequences of ignoring gender and biology in Alzheimer’s disease is absent from the political dialogue. In 2020 Alzheimer’s and other dementias will cost the US $305 billion, and these costs are likely to keep rising without immediate action. While the fight to find a cure is as important as ever, one of the most significant ways to save lives is by preventing Alzheimer’s disease in the first place.
Investing in research that looks across a woman’s lifespan to identify risk factors for Alzheimer’s disease and related dementias can help women monitor early warning signs and potentially mitigate risk factors that can prevent or delay the onset of cognitive impairment. This research has the potential to save millions of lives that would otherwise be lost to Alzheimer’s, and to significantly reduce the hefty price tag that Alzheimer’s disease and related dementias presents for patients, families, caregivers and our healthcare system.
Scientists are discovering more about the risk factors and warning signs of Alzheimer’s, particularly in women. While the devastating diagnosis of Alzheimer’s disease is often a shock for patients and their loved ones, the reality is that for most, Alzheimer’s and related dementias don’t appear out of nowhere. In fact, for women, we can begin identifying these risk factors early in life.
New promising research shows that there are unique, sex-specific risk factors that contribute to Alzheimer’s disease risk in women that scientists and clinicians can begin to identify at earlier stages. Examples of these risk factors include hypertensive pregnancy disorders and the removal of both ovaries before natural menopause. In addition, the relationship between lifetime use of contraceptives and/or menopausal hormone therapy and subsequent risk of Alzheimer’s disease, is not known.
Building on these gaps, studies at the Mayo Clinic are developing a more complete tool for assessing a woman’s risk of Alzheimer’s disease by developing a “lifespan” approach to identifying and understanding risk factors across a woman’s entire life that could indicate her subsequent risk of Alzheimer’s disease and related dementias. Understanding the sex- and gender-specific causes of Alzheimer’s disease can help tailor treatments and mitigation strategies to each individual. Conducting and investing in broad lifespan research can also help to develop risk assessment tools that paint a more accurate picture of any given woman’s Alzheimer’s risk.
Transitional moments like pregnancy and menopause are the functional equivalent of a “stress test” on the body and the brain. Although all women go through menopause and many women become pregnant, not all women develop Alzheimer’s diseases and other dementias. Observing how the body responds to the significant transitions during pregnancy and over the menopause transition, including hormonal, inflammatory, and other changes, could provide critical insight to subsequent disease risk. For example, women who develop elevated blood pressure during pregnancy, that then subsides, experienced more dramatic cognitive decline and greater brain atrophy decades later when compared to women with normal blood pressure throughout pregnancy. More than one in seven women experience elevated blood pressure, or hypertension, during a pregnancy over the course of their reproductive period so a large number of women are affected and at increased risk of cognitive changes.
Moments like these are critical opportunities for clinical interventions. While there is not yet a cure or treatment for Alzheimer’s disease, there are effective treatments for many of the underlying conditions that can elevate one’s risk for Alzheimer’s down the road. Treating the immediate health issue, like increased blood pressure during pregnancy, is both an opportunity to take preventative action as well as a warning sign that one should monitor risk going forward.
Given the potential for sex- and gender-based research, one might expect clinical research to account for differences between men and women and, at a minimum, include women in parity. But this is not the case. Roughly two thirds of animals used in neurodegenerative research are male or of unreported gender, meaning sex isn’t even considered as a variable. In fact, it wasn’t until 1993 that the FDA mandated that federally-funded clinical research even include women and pharmaceutical companies and device manufacturers to this day are not required to comply with this rule. Making sure females are included and considered in research that so directly and differentially impacts women is critical to making progress in Alzheimer’s research and related dementias. It’s also just good science.
For generations many have accepted Alzheimer’s as a tragic, yet inevitable, price of aging. But, it doesn’t have to be this way. Now, a growing body of scientific evidence around dementia risk-reduction strategies makes clear the need to invest in brain health and sex-based research across the lifespan. By targeting interventions that factor in biology and gender, we will not only slow disease progression and bolster our economy, but the biggest payoff will be to offer millions of women and men a more productive and extended quality of life.
Carolee Lee is CEO and Founder of AccessCircles and WHAM! (Women’s Health Access Matters), a nonprofit organization bringing private investment, coordination, and attention to accelerate gender-based research.
Michelle M. Mielke is a Professor of Epidemiology and Professor of Neurology, the Co-Director of the Specialized Center for Research Excellence on Sex Differences at Mayo Clinic, and is an expert in sex-specific differences in the risk and progression of neurodegenerative diseases.
Being Patient is committed to representing a diversity of voices in the Alzheimer’s and brain health community, and to providing a platform to elevate the perspectives of people living with neurodegenerative diseases. Being Patient publishes op-eds at the discretion of the editorial staff. To share an op-ed for consideration, submit concepts or drafts to our managing editor at alex@beingpatient.com.