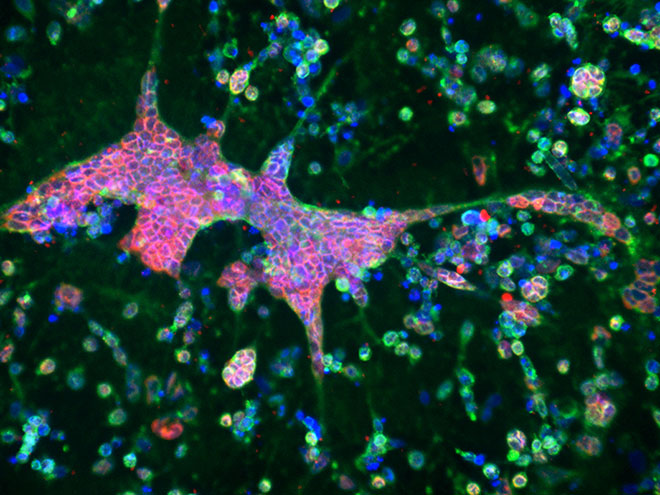
A six-millimeter-wide, donut-shaped sponge made of silk protein and collagen, populated with neural stem cells, can now show scientists exactly what it looks like when herpes hastens the onset of Alzheimer's.
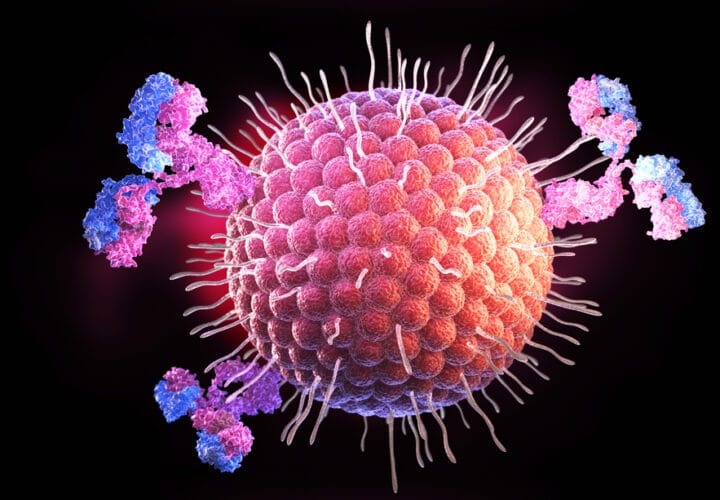
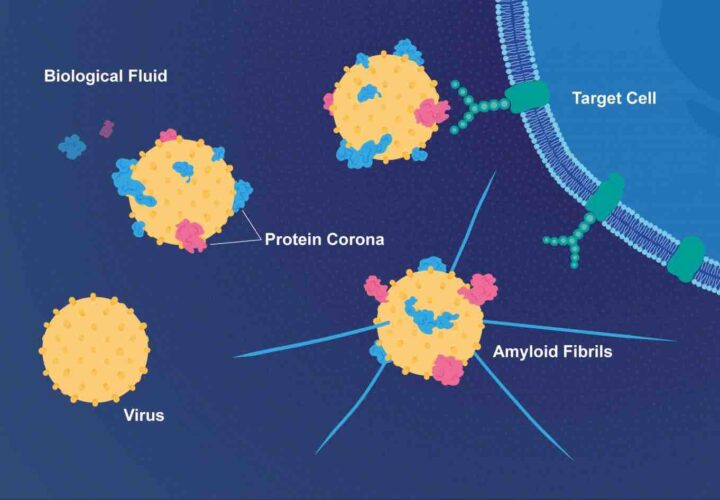
A 2018 study found that herpes is linked to half of all Alzheimer’s cases, but it wasn’t clear why. Then, a year ago, a mice study concluded that Herpes simplex 1 (HSV-1), along with other viruses, can speed up the development of neurodegenerative diseases like Alzheimer’s, as their protective layer of proteins bind to beta-amyloid proteins in the brain. These proteins drive the formation of the brain plaques and tangles that are understood to cause types of dementia.
Now, researchers at Tufts University have created a 3D brain tissue model of what they call this “potential causal relationship” in action, allowing them to dive deeper into what happens when a virus like herpes begins interacting with the brain.
“After just three days of herpes infection, we saw large and dense plaque formations of beta amyloids, as well as increased expression of some of the enzymes responsible for generating the plaques [that can cause Alzheimer’s],” said David Kaplan, professor and chair of the Department of Biomedical Engineering at Tufts’ School of Engineering. “We observed neuron loss, neuroinflammation and depressed signaling between neurons — everything we observe in patients. Never before have so many facets of the disease been replicated in vitro.”
By “in vitro,” Kaplan is referring to the stem-cell sponge-donut — or the tissue model — in which his lab has been able to observe physical and biological changes in the neurons in real time and monitor electrical activity between the cells as they communicate. The model is designed to study the origins of diseases using genetically normal cells — a clearer option than previous models have achieved.
In part, models like this one can help provide information critical to screening experimental drugs designed to either prevent or mitigate Alzheimer’s at its earliest onset.
For example, Kaplan’s tissue model allowed Tufts researchers to view the real-time effects of valacyclovir — one of a number of FDA-approved antiviral medications used to treat the severity and frequency of herpes symptoms — as it rolled back some of the effects of herpes that might otherwise lead to Alzheimer’s.
The researchers also learned from the model that in the brain tissue infected with the herpes virus, 40 Alzheimer’s-associated genes were over-expressed, some of which are linked to the production of the beta-amyloid peptides found in plaques.
The researchers said that some of these 40 over-expressed genes could be new targets for developing future Alzheimer’s drugs.
For further reading on the link between Alzheimer’s and herpes, Dr. Rudy Tanzi takes a deeper dive into his research for Being Patient in a 2018 BrainTalk.