Here's a closer look at a kind of dementia that often causes loss of speech — primary progressive aphasia — and how Alzheimer's biomarkers may play a role.
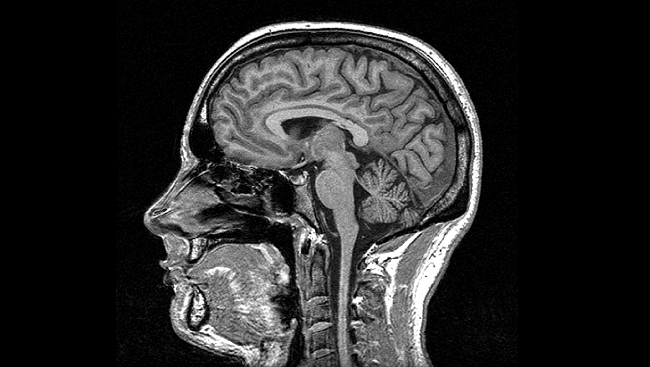
A new study shows that individuals with a neurodegenerative language disorder called primary progressive aphasia (PPA) have Alzheimer’s-like plaques and tangles in their brains — but no associated memory deficits. The 2022 study, published in the journal Neurology, adds to the mounting evidence that these plaques and tangles may be able to exist without the memory decline in Alzheimer’s. The researchers took a close look at a neurodegenerative brain disease — a type of frontotemporal dementia — called primary progressive aphasia.
Primary progressive aphasia is one of a couple major forms of frontotemporal degeneration (FTD), which affects the brain in ways that impact communication: language skills, speaking, writing and comprehension. Most typically, this appears in midlife, before age 65.
What is Primary Progressive Aphasia?
Primary progressive aphasia is a blanket term for a group of neurodegenerative diseases characterized by language impairment, and associated with Alzheimer’s. Like Alzheimer’s, it is also fatal and incurable, and it also affects mostly older adults.
The participants in the study included 17 people with primary progressive aphasia associated with Alzheimer’s, and an additional 14 people who exhibited the traditional Alzheimer’s condition with memory deficits. Participants were then compared in two ways: memory tests and brain scans and, eventually, autopsies.
Traditional memory tests involve the use of verbal skills, like remembering word-pairs. These verbal skills are significantly affected in people with primary progressive aphasia. M. Marsel Mesulam, from the Northwestern University Feinberg School, an author of the study and a Fellow of the American Academy of Neurology, explained in a news release, “[Memory] has been difficult to determine, because most memory tests rely on verbal skills that these people have lost or are losing.”
What did the study find about Alzheimer’s biomarkers in PPA?
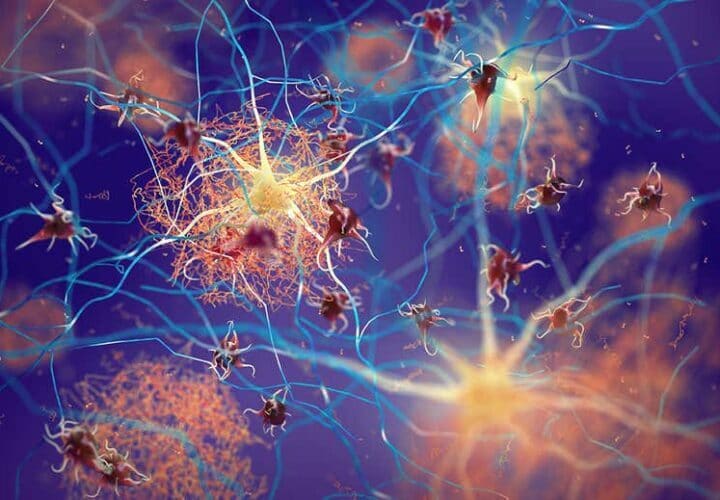
The increased incidence of beta-amyloid plaques and tau tangles in the brain has been long thought to be the underlying cause of Alzheimer’s disease. However, the research community’s trust in this theory has diminished in recent years, as experimental Alzheimer’s treatments targeting beta-amyloid experience failure after failure. One problem is that between 20 and 40 percent of people aged 70 and up have beta-amyloid plaque deposits in their brains but do not have dementia.
Meanwhile, studies have found it is also possible to have dementia without Alzheimer’s hallmark beta-amyloid plaques. If research can rule out protein plaques and tangles as the driving force behind the cognitive changes associated with Alzheimer’s, scientists can better identify drug targets to treat the disease, expediting the search for a cure.
The new study found that some people with a particular language disorder, primary progressive aphasia, who also had hallmark proteins of Alzheimer’s in their brains, did not exhibit the memory deficiencies commonly linked with the disease.
In a clever work-around, the participants with primary progressive aphasia were given a memory test involving the remembering of objects, rather than words. Their performance in this task was contrasted with the performance of individuals with Alzheimer’s without aphasia, in a traditional memory test.
When these tests were repeated a few years later, participants with primary progressive aphasia showed no decline in memory, even though they had suffered from the condition for an average of six years. However, their language skills declined drastically. On the other hand, for people with the typical Alzheimer’s condition, both language and memory declined consistently.
Particularly interesting were the brain scans, which showed a comparable presence of beta-amyloid plaques and tau tangles in the brains of participants in both groups.
The researchers attributed these conflicting findings, in part, to the lower prevalence of Alzheimer’s-hallmark brain proteins known as ApoE4 and TDP-43, surmising that decreased levels of these proteins could be linked with the preservation of memory.
The strength of the findings is limited by the small sample size, and Mesulam calls for further investigation. “More research is needed to help us determine what factors allow these people to show this resilience of memory skills even in the face of considerable Alzheimer’s disease pathology in the brain,” he said.