Two years after a COVID-19 infection, adults aged over 65 may be more at risk of developing dementia and other cognitive disorders.
According to experts, we may be living through one of the greatest mass disabling events in history — the COVID-19 pandemic. Studies analyzing the post-infection impact on cognition compared the infection’s effect on the brain to 20 years of aging, reporting a broad range of worrying symptoms that include brain fog, memory impairment and difficulty focusing. How long did these symptoms last — and could they open the door to more serious cognitive problems down the line
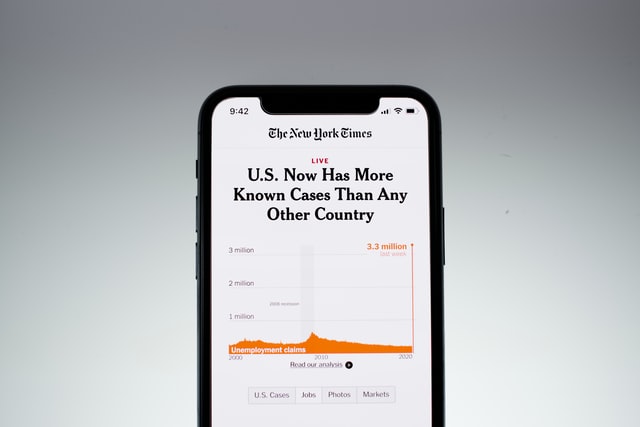
Researchers at the University of Oxford published a new study in The Lancet Psychiatry which tracked post-COVID risk over the course of two years in 1.2 million people. The results were alarming, showing that, for a certain subset of people who recovered from COVID-19 two years ago, the chances of developing dementia rose from a 10-percent chance to a 13-percent chance — a one-third increase — along with statistically significant higher risk for other cognitive issues, from seizures to psychotic disorders.
These findings add to other recent research on the downstream cognitive repercussions of COVID-19 infections. Another study found no difference in the risk of developing Alzheimer’s when compared to other individuals recovering from other respiratory infections after one year. They also found that COVID-19 and other respiratory infections tripled the risk of receiving an Alzheimer’s diagnosis within the following year. While the results seem at odds, the latter study did not assess the risk of developing Alzheimer’s or any other dementia after two years. It is possible that COVID-19 has more of a lasting impact on brain health than other respiratory infections.
Children and adults younger than 70 didn’t seem to share any long-term cognitive impacts two years after their initial infection with the virus. But the findings were different for adults 70 or older. In the older group, the risk of cognitive deficits was significantly higher compared to adults of the same age who did not have COVID-19.
Paul Harrison, professor in Oxford’s department of psychiatry, led the research.
“It is worrying that some other disorders, such as dementia and seizures, continue to be more likely diagnosed after COVID-19, even two years later,” Harrison said in a press release. “It also appears that omicron, although less severe in the acute illness, is followed by comparable rates of these diagnoses.”
What did the study find?
The researchers accessed records through an electronic health database to compare people recovering from COVID-19 to a control group of people who were recovering from another type of respiratory infection. Tallying up the frequency of 14 psychiatric diagnoses, they could then determine whether a COVID-19 infection increased the risk compared to the control group.
After two years, older adults still showed a 36-percent increase in the risk of developing a cognitive deficit, a 33-percent increase in dementia risk, a 14-percent increase in developing epilepsy or seizures and a 27-percent chance of developing a psychotic disorder.
What exactly do these percentages mean?
It is important to consider that the risk of developing dementia is linked to age, and to risk factors like genetics and lifestyle. Ten of every 100 people over 65 will develop dementia. For people 65 or older who were infected with COVID-19, this number rises to 13 of every 100 — and that’s approximately one third more risk for each individual, from a 10-percent to a 13-percent chance of dementia in their lifetime..
“Even though some variants may have been deemed ‘milder’ in their impact on people during infection, the longer-term consequences of infection appear to be similar regardless of variant,” said Rachel Sumner, PhD, a senior research fellow at Cardiff Metropolitan Hospital who was not involved in the study. “This is even more concerning for those that work in frontline roles, who are exposed to COVID-19 infection repeatedly with very little ability to keep themselves safe from it.”
COVID-19 is Bad News for Brain Health
The study presents compelling evidence that COVID-19 infection may have repercussions for brain health, even two years after the initial infection.
There are limitations with these studies that are challenging to resolve without traveling into the future to see how long these risks last or if they increase the severity of dementia later in life.
The study also does not tell us whether these diseases were already present before a COVID-19 infection. But it does strengthen the link between the immune system, post-viral disease, and Alzheimer’s.
Already, there is evidence that vaccines against infectious diseases reduce the risk of developing dementia, as well as several efforts underway to develop an Alzheimer’s vaccine.
“The findings shed new light on the longer-term mental and brain health consequences for people following COVID-19 infection,” Dr. Max Taquet, the first author on the study said in a press release. “The results have implications for patients and health services and highlight the need for more research to understand why this happens after COVID-19, and what can be done to prevent these disorders from occurring, or treat them when they do.”