In Being Patient’s LiveTalk series, Dr. David Weidman, associate medical director for research at the Banner Alzheimer’s Institute, shares insights on Eli Lilly’s investigational Alzheimer’s drug donanemab, discussing the drug’s trial data so far, and its effects on Alzheimer’s symptoms and key biomarkers of the disease.
Just a few weeks after the Food and Drug Administration approved Biogen’s Alzheimer’s therapy Aduhelm, Eli Lilly’s investigational drug donanemab, also designed to treat early-stage Alzheimer’s, earned the agency’s breakthrough therapy designation, which aims to accelerate the development and review of drugs for serious conditions.
Being Patient spoke with Dr. David Weidman, associate medical director for research at the Banner Alzheimer’s Institute and principal investigator of two donanemab trials, about donanemab’s similarities and differences compared to Aduhelm, as well as his read on new results from donanemab’s Phase 2 clinical trial.
(In February 2024, Biogen took Aduhelm off the market indefinitely.)
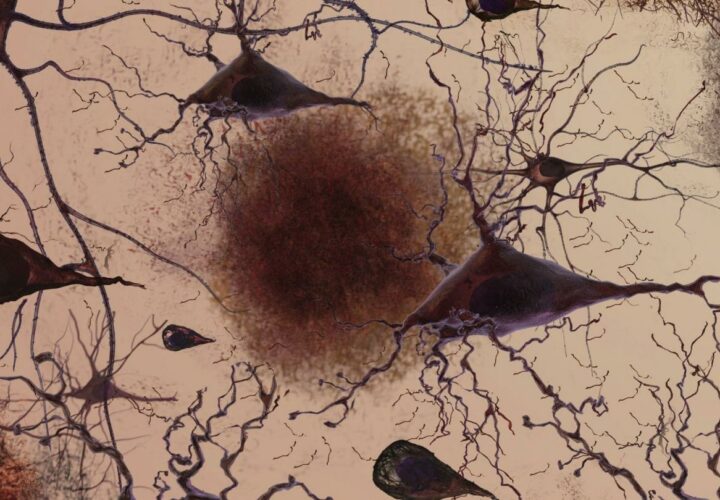
Dr. David Weidman: Yes. They’re both MABs, which is an acronym for monoclonal antibodies. They both target parts of this fibrillar or solidified or insoluble amyloid plaque in the cortex of the brain. I liken that to if you leave bread in the toaster too long, then the outside of the bread gets crusty.
Aducanumab, now branded as Aduhelm, targets different parts of this fibrillar, solid amyloid in our cerebral cortex or surface of the brain. Donanemab attacks a very specific part of the protein called N3pG, which is an epitope, along an amino acid chain, whereas aducanumab is fully humanized.
[Aducanumab] was derived from antibodies made by very elderly folks who didn’t get Alzheimer’s. Fifteen, 20 years ago, someone had the bright idea [to] — through all of the genetic engineering — amplify actual antibodies made by elderly folks that were cognitively resilient, whereas donanemab is not fully humanized, but [it is] humanized, meaning it was originally tested and synthesized in animals and then it’s modified so the human body doesn’t create an allergy when exposed to it.
Being Patient: Can you share with us some of the results from donanemab’s clinical trials?
Dr. David Weidman: Donanemab clearly, clearly has an interesting mechanism in that it lowers the amyloid burden and gets it out of the brain and into the circulation promptly to almost normal levels, such that in this Phase 2 trial, about a quarter of patients within six months had a lowering of amyloid. We didn’t even know they could be switched to placebo because the drug already did its job. Then after about 12 months, about half of the folks had amyloid sufficiently removed. Mind you, it’d be nice to see this replication in the Phase 3 trial.
Now of course, the caveat here is we don’t know the duration of that lowering or removal over the expected duration of Alzheimer’s disease, but it certainly is something we need to think about in terms of feasibility and practicality that this drug could be given at an early-stage for only a year while we think about a cocktail [of treatments] or other things to do.
Want to learn more about clinical trials
for Alzheimer’s and dementia?
Check out the Lilly Trial Guide.
Being Patient: Scientists are also studying the effects of treating tau pathology, another Alzheimer’s hallmark.
Dr. David Weidman: There is increasing research, even within these trials, to understand whether or not if given early enough, anti-amyloid therapies lowering the cortical amyloid will somehow then lead to slower accumulation of the other protein that defines Alzheimer’s: The tangles which are inside the cell. Cell death and loss of synapses with the further accumulation of the tau or tangles is much more closely associated with symptoms. The amyloid plaques start collecting 10 [years], and in genetic cases sometimes 15 to 20 years, before symptoms even begin.
Being Patient: What do we know about donanemab’s effects on tau?
Dr. David Weidman: Within the donanemab trial, which was Phase 2 [and] although small [in] numbers, there is some evidence that in specific regions of the brain where the tau seems to collect in a greater fashion — because it seems to propagate along a certain pathway, mainly the temporal lobes — that there is some slowing down of accumulation of that tangle burden, or tau burden, in the treatment group. That’s fairly exciting and does lend credence to the fact that there can be some disease modification from anti-amyloid antibodies.
The donanemab trial was really the first Phase 2 trial to meet a clinical endpoint, which is above board and published in The New England Journal of Medicine in March of this year. That of course generated some excitement and a transition to Phase 3 of much larger numbers based on some encouraging findings from Phase 2.
Being Patient: A heavier burden of tau can indicate that a patient is in the later stages of Alzheimer’s. Is that correct?
Dr. David Weidman: Yes. The amount of tangle or tau deposition is more closely associated with symptoms, but [also] helps define what stage one is in within the whole continuum [of Alzheimer’s]. For arbitrary reasons, we say cognitively unimpaired, mild cognitive impairment, and then [mild, moderate and severe stages of Alzheimer’s], but they’re really not discrete entities. It’s a continuous process. We might have a better way to refine [the answers to the questions of ‘is the patient] in early mild cognitive impairment? Is the patient in late mild cognitive impairment? Are they about to lose their independence? Do they already have mild-stage Alzheimer’s?’
Being Patient: One of the main side effects of anti-amyloid therapies is amyloid-related imaging abnormalities (ARIA). Can you tell us more about ARIAs in donanemab’s Phase 2 trial?
Dr. David Weidman: Years ago, it was considered a side effect. Now, it’s an effect and it’s expected in a certain number of people [treated] with these types of antibodies, especially as you go up in therapeutic doses, there can be upwards of 20 percent to 40 percent of people [who] may actually have [an] effective reaction, where amyloid [is cleared] into the blood vessels on the top of the brain cortical. That whole process makes that part of the brain a little leaky or more porous, depending on where the amyloid is greatest in its load or accumulation. It can have two reactions. One is moving [amyloid] out will lead to a little leakage of water either on the surface of the brain or just underneath the surface of the brain.
Or, the increased porous nature of the whole process can lead to a little leaking of this mobilized amyloid into vessels, and they do penetrate the brain to give oxygen. Sometimes, these blood vessels are inside the brain. These are called microhemorrhages or microbleeds, little iron deposits.
The rate of the watery type [of] ARIA (edema) was six percent with donanemab in terms of causing symptoms of headache, confusion, dizziness. But we’ve learned over the last 10 or 15 years to [monitor for ARIA and to quickly hold] the dose, letting the edema or water resolve. If there [are] too many microbleeds, that means the person may also have amyloid in their blood vessels to begin with. Then sometimes if [patients] accumulate too many microbleeds, we’re worried about a bigger hemorrhage and we just have to stop the drug permanently in those trial participants.
There was no macrohemorrhage in the [Phase 2 trial of] donanemab. The incidence of that was very low with aducanumab. There were a couple of persons with stroke-like symptoms in the Phase 2 [trial] of donanemab, which did reverse.
Being Patient: Like Aduhelm, donanemab is by no means a cure, right?
Dr. David Weidman: [Donanemab treatment for] the earliest symptomatic stages of Alzheimer’s can only go so far to slow down decline about 30, 35 percent. It’s a huge start and it [has] really generated enthusiasm, as of course has Aduhelm, but it does not improve day to day symptoms. An individual patient is going to have to have these infusions on faith that it will slow down decline.
[Donanemab is] certainly not a cure. In fact, the Alzheimer’s field really doesn’t have trials to halt or reverse years. Our first goal in disease modification — and it’s of course a big hurdle before we get to [trials to halt or reverse Alzheimer’s progression] in the future — would be to slow down cognitive and functional decline.
The interview has been edited for length and clarity.
Contact Nicholas Chan at nicholas@beingpatient.com
UPDATE: 3 March 2024, 9:01 P.M. ET. In February 2024, Biogen took Aduhelm off the market, citing financial concerns. Although the drug did receive accelerated, conditional FDA approval for the treatment of early Alzheimer’s disease in 2021, it is no longer available to new patients. The company announced it would sunset trials in May 2024 and cease supplying the drug to current patients in November 2024.

When a drug be on the market for dementia, in the next two years?