This article was produced by Being Patient in partnership with Charter Research. More information on Alzheimer’s clinical trials can be found on the Charter Research Website.
Some people complain of mental fogginess after COVID-19. As new research and therapies emerge, what new insights can we learn about the brain?
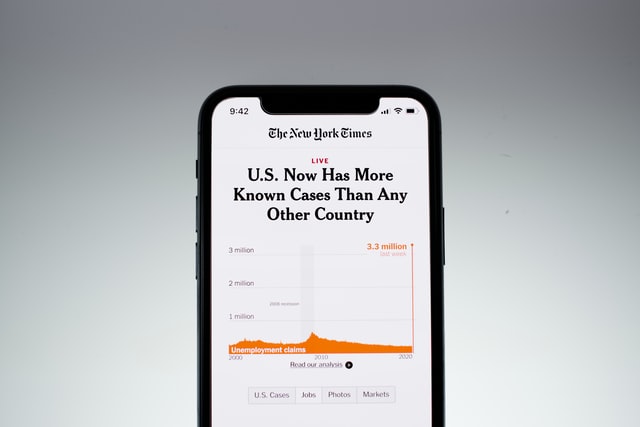
Right around this time one year ago, the CDC announced that SARS-CoV-2, the virus responsible for COVID-19, was heading toward pandemic status. We’ve learned much about the virus since then, but when it comes to long-term effects, there are still many questions left unanswered. Take for instance, brain fog, a collection of neurological symptoms including confusion, foggy thinking, trouble making decisions and memory issues that afflicts many virus sufferers both during and after the infection. Currently, there are no treatments to alleviate brain fog attributed to COVID-19. While scientists still don’t have answers for why some people develop these symptoms and others don’t, they are starting to understand what causes this cognitive impairment and what therapies work to alleviate symptoms.
Although brain fog isn’t considered an official medical term, it is a serious phenomenon. Dr. David Nauen, assistant professor in the department of pathology at Johns Hopkins University in Baltimore, compared the cognitive condition to the way you feel when you’re tired, and your ability to process information lags.
“One is unable to form thoughts as precisely and often not able to access the information in the brain with the same ease that is normally there,” Nauen told Charter Research. “It can be pretty dramatic for people and have a severe effect on not only the subjective sense of well-being, but also on things like the ability to earn a living.”
He said that when the pandemic first hit, he along with other neurological specialists were confident that COVID-19 affects the brain, knowing what they do about other viruses (Herpes Simplex virus and West Nile virus) that attack the brain and pose often severe neurological consequences. But to his surprise, the signs of a viral impact on the brain — for example, inflammation or white blood cells — were absent in COVID patients.
“We had this mystery, with people having a lot of neurologic problems and many reports that there was something going on in the brain, yet, on the other hand, there was very little inflammation and essentially, there was no virus,” Nauen said.
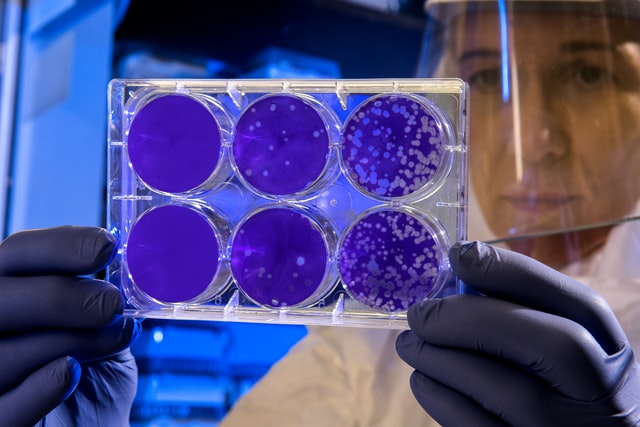
Decades ago, the only way to confirm an Alzheimer’s diagnosis was by performing an autopsy on the brain. Now, experienced physicians can correctly diagnose the disease with 90 percent accuracy, while the person is still alive. As the medical community navigated COVID-19’s uncharted waters, autopsies proved to be one of the best ways to get a better understanding of the virus. However, during the first few months of the pandemic, Nauen wasn’t able to perform autopsies on the brain due to the risk of exposing himself and his team to the virus through aerosolization from the postmortem procedure. After a few months, he took to a more antiquated approach, using hand tools to access the skull to reduce particles in the air.
At first, Nauen didn’t see any abnormalities. But as he looked more closely through a microscope, he started to see large cells. “It was really strange. For a minute or two, I was just like, what are these? I’ve never seen anything like that in the brain before. Then I realized that they were megakaryocytes.”
Megakaryocytes (mega meaning large, karyocyte meaning any cell that possesses a nucleus) are very large cells with huge nuclei, involved in making platelets in the bone marrow, which are necessary for blood clotting. These megakaryocytes were found in the brain’s thin blood vessels, known as capillaries, which bring oxygen to the brain. “It’s just really out of place to see them in the brain. It would be like being onstage and looking out at the audience and then suddenly seeing a dog sitting in a leather seat instead of a human being,” Nauen said.
Nauen and his team found megakaryocytes in one-third of the brains they surveyed, but he expects their presence is more prevalent than that. “The fact that we saw these cells on these totally random sections almost certainly implies that there are a lot of others that we did not see, because we didn’t examine the whole brain,” Nauen said. They also offered a clue about the prevalence of brain fog.
“All these lines of evidence point to possible altered delivery of oxygen and then possibly altering pressure within the vascular system of the brain, which could contribute to brain fog and could even increase the risk of stroke,” he said. “Over the past couple months, other papers have come out showing megakaryocytes in the lungs, kidneys and the heart. They [megakaryocytes] could be contributing to these really difficult COVID-19 side effects like brain fog.”
As the medical community continues to search for answers about where these cognitive difficulties stem from, other researchers have set their sights on treating the symptoms at hand. A new clinical trial at the University of Alabama at Birmingham (UAB) draws on a rehabilitation method that has proven successful in treating patients with stroke, multiple sclerosis, traumatic brain injury and cerebral palsy to combat brain fog or continued cognitive issues caused by COVID-19.
In collaboration with colleagues at UAB, Dr. Edward Taub and his longtime research partner Dr. Gitendra Uswatte have developed a method for improving cognitive impairment in the laboratory in a way that helps patients more seamlessly transition back to normal life. The method, called Constraint-Induced Movement therapy (CI therapy), consists of a family of treatments that teach the brain to ‘rewire’ itself following an injury to the brain. The initial techniques were tested on monkeys who had lost sensation in one of their four limbs. Taub discovered that constraining their good arm by strapping it to the side of their body incentivized the usage of the weaker arm, ultimately strengthening not only the muscles in the arm, but also the brain.
“The brain is a very plastic organ,” Taub said. “If you start using a function more than you had been, the part of the brain that innervates that function increases in size. The opposite occurs if you stop using a part of the body. For example, if you put a leg in a cast, that person can’t use the leg so the part of the brain that supports or innovates movements of the leg shrinks over a period of just 10 days.”
Over the years the technique has proved greatly successful in humans. In a study with thousands of stroke patients, about 97 percent saw meaningful improvement in their symptoms post-treatment and on average, the patient reported using his or her affected limb five times more post-therapy than pre-therapy. MRI scans have also shown significant brain rewiring in just two weeks of intense clinical training, according to Taub. This has since convinced the pair that CI therapy could improve cognitive impairment following COVID-19 infection.
“It doesn’t matter where the damage is to the brain and what type of specific damage it is, those principles still apply,” Uswatte said. “That’s one reason why we think the CI therapy is going to apply to people with brain fog from COVID-19.” Another reason for their confidence stems from their success in treating people who have had strokes. Knowing that a subset of COVID-19 patients experience strokes, they are confident the therapy will translate well.
“We use exactly the same techniques and strength, not restraint, but constraint,” Taub said. “That is, we don’t permit the patient to do what a person with aphasia (difficulty communicating) normally does to communicate with others. Typically they won’t speak and will just gesture and grimace. They get other people like family members to do the task or to speak for them. We prevent that and we encourage the caregiver to not to speak for the patient so that they do it themselves.”
Taub and Uswatte are currently recruiting for the trial, which will include at least twenty adult patients who have recovered from COVID-19 and are experiencing cognitive issues. Each participant will undergo 35 hours of therapy in a clinic, spread over two weeks’ time and will have individualized homework assignments based on their individual needs.
While full results will only be available in Fall 2021, they’re already seeing positive signs the therapy is working. Their first patient is only about a third of the way through treatments and has already made substantial improvements, similar to how their patients with cognitive impairment have after stroke, according to Taub.
All three doctors strongly believe vascular health is intimately connected to the brain. “Things like hypertension, high blood pressure and poorly controlled blood sugar for diabetics can be so devastating to brain function and there are a lot of studies that suggest those factors could be increasing the risk of Alzheimer’s disease,” Nauen said. “Vascular health is really critical for brain health.”
Uswatte echoed Nauen’s theory, stressing that evidence points to a connection between COVID-19 and the vascular system.
“There are other types of damage that we’re still learning like vascular [damage],” Nauen said. “A subset of COVID long haulers have damage to the vasculature in their limbs, particularly lower limbs. They have an inadequate return of blood flow to their heart, which means there’s less blood going to organs all around the body, including the brain.”
What these findings mean for neurodegenerative diseases like Alzheimer’s remains to be seen. Taub and Uswatte said they’re interested in seeing if CI therapy works for people with neurodegenerative disorders like Alzheimer’s. “If we get a positive result [from the brain fog trials], it would certainly increase our interest in then applying the intervention to people with Alzheimer’s disease.”
Contact Genevieve Glass at genevieve@beingpatient.com