Both COVID-19 survivors and people who have not to their knowledge been infected with SARS-CoV-2 are experiencing cognitive symptoms widely referred to as “brain fog.”
Neuroscientist Kristen Willeumier, PhD, author of Biohack Your Brain, and neurologist Dr. Majid Fotuhi, author of Boost Your Brain, help us understand why we shouldn’t disregard COVID-19 “brain fog,” and what works best to get back on track.
It is hard to believe it’s been a year since SARS-CoV-2, the virus responsible for COVID-19, was first detected in Wuhan, China. During this pandemic, we have become all too familiar with the seemingly endless list of symptoms associated with the disease – fever, shortness of breath and dry cough, to name a few. But often the most frustrating symptoms are invisible to the eye and persist long after the acute phase of infection. Take for instance, brain fog – a collection of neurological symptoms that afflicts many virus sufferers both during and after infection.
Because “brain fog” is a colloquial term rather than a medical one, it is often avoided by physicians and patients alike. Being Patient taps into the knowledge and expertise of two neurologists to understand why we must pay attention to the syndrome, as well as what works best to lift the fog.
Dr. Majid Fotuhi, a Harvard and John Hopkins trained neurologist and neuroscientist, describes brain fog as an all-inclusive term that encompasses the inability to concentrate, increased absent mindedness, difficulty recalling or retaining information, fatigue, insomnia and changes in mood. There is no test or measurement to access brain fog, nor is it considered an official medical diagnosis. On top of all that, it’s difficult to predict who is at risk and what percentage of COVID-19 patients may experience it.
As one goes through early stages of development, childhood and teenage years, they’re constantly making new synapses – a lot more than they need – which contribute to their cognitive reserve. “The synapses are like money in the bank, and you don’t use most of them during your day-to-day life. The wear and tear of aging, as well as medical conditions, reduce the number of synapses in our brain,” Fotuhi explains. While young people are certainly not immune to coronavirus related brain fog, this explains why older people generally experience worse cognitive symptoms, from brain fog to mood changes to more extreme neurological symptoms like paralysis. The higher one’s cognitive reserve, the more resistant their brain is to any dysfunction that comes their way.
Comorbidities impact cognitive reserve, too. In general, Fotuhi said, “People who have a mood disorder or preexisting medical conditions such as diabetes, obesity or heart failure are more likely to develop symptoms if they are infected due to a slightly lower cognitive reserve.”
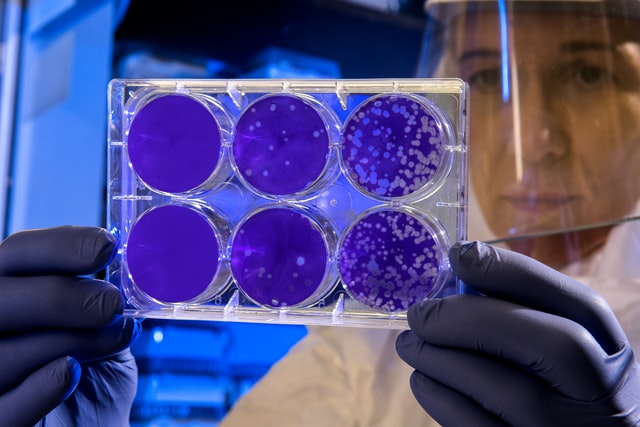
The Novel Coronavirus and the Immune System
Fotuhi added that there is mounting evidence that, when it comes to COVID-19, the culprit for neurological symptoms is not the virus itself, but rather our immune system’s overzealous response to it.
The spike protein of the virus, usually called the S1 protein, is the key driver that helps the virus cross the blood-brain barrier, contributing to neurological symptoms, like brain fog. This binding protein often detaches from the virus, causing the brain to release an exaggerated cytokine response, triggering widespread inflammation and wreaking havoc on the nervous system. “This excessive inflammation affects the brain, heart, kidneys, liver and every other organ,” Fotuhi said.
“There are few known infectious agents that have caused such a huge immune response as COVID-19, which is surprising,” he added. “It’s a very little virus with very few genes and proteins but causes a bomb to the immune system.”
Kristen Willeumier, PhD, a neuroscientist with extensive research expertise in brain function, points to another common symptom, loss of smell, as another way to see how the virus affects the brain: “COVID-19 has neurological symptoms because it can get in through the body through the oral mucosa, the eyes and the nasal epithelium. Loss of smell and taste is frightening,” she said. This symptom could mean that the virus is affecting olfactory neurons or the olfactory bulb, the system devoted to our sense of smell, all residing in our brain.
Now, back to brain fog: Willeumier says another reason for mental fuzziness could be attributed to “low levels of oxygen circulating throughout the brain and body during the virus.” Decreased oxygen levels fiercely impact our brain tissue, which can lead to confusion or worse, a coma or permanent brain damage. A recent NYU study found that 606 out of 4,491 COVID-19 hospitalized patients developed a neurological disorder within two days of symptoms starting.
Fotuhi also urges these patients to get a cognitive evaluation to understand how their mental faculties compare to others in their age group – the recommended score should be around the 50th percentile. Anything under the 10th percentile warrants a trip to the neurologist.
Fotuhi said hospitalized coronavirus patients who experienced any distressing neurological symptoms at all, even headaches, should undergo a brain MRI to determine if a stroke of any size has occurred. Fotuhi also urges these patients to get a cognitive evaluation to understand how their mental faculties compare to others in their age group – the recommended score should be around the 50th percentile. Anything under the 10th percentile warrants a trip to the neurologist.
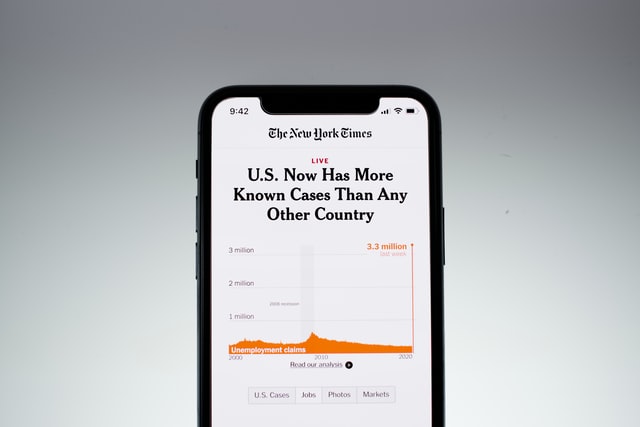
According to Willeumier, the brain fog isn’t limited to coronavirus patients. “We’re experiencing brain fog more and more due to the stress of the coronavirus. Not just the people who get the virus, but people who don’t,” she said. “We are collectively bombarded by media messages instilling fear around the coronavirus, including telegraphing the numbers of people dying, the new mutating strands, the vaccine… The messaging, which is repeated day in and day out, is enough to cause a stress response in the brain and the body which can lead to brain fog.”
Clearing the Haze
It’s not all doom and gloom. Both doctors agree that although we don’t know what the long-term consequences will be, it is important to recognize that the neurological symptoms due to COVID-19 are treatable.
As the medical director of NeuroGrow Brain Fitness Center, Fotuhi said he has seen up to a 90 percent success rate for concussion patients during his 12-week brain rehabilitation program, which includes brain training, neurofeedback and lifestyle interventions. He is applying these same, multidisciplinary therapeutic approaches to help COVID-19 patients recover lost cognitive capacity.
If you don’t have access to a center like this one, don’t fret. Most of these practices are easy to implement at home. Fotuhi said learning new things, exercising, sleeping eight hours a night and meditation for stress reduction are the main ways to combat brain fog and further enhance your cognitive reserve. He assures following this protocol diligently will produce results within a month.
“We’re experiencing brain fog more and more due
to the stress of the coronavirus. Not just the people who
get the virus, but people who don’t.”
In addition to these strategies, Willeumier believes good nutrition is crucial to supporting mood and memory health. She recommends following a Mediterranean diet, which consists of vegetables, fruits, whole grains, legumes, fish and of course, extra virgin olive oil. “This way of eating helps protect the brain from cardiovascular and neurological disorders, which is shown in evidence-based literature,” she explained. Because many of our diets don’t have enough of the vitamins, nutrients and minerals and enzymes we need to maintain our brain health, calling on supplements is another way to help fortify and protect brain function.
Regardless of what diet you follow Willeumier recommends taking the following supplements: omega-3 fatty acids, a high-quality multivitamin, Vitamin C, Vitamin D, zinc, probiotics and curcumin a.k.a. turmeric, to name a few. “Curcumin, which comes from the root of the turmeric plant is an amazing anti-inflammatory, not just for the body, but for the brain. Certain forms of curcumin can actually cross the blood brain barrier and bind to the plaque that can lead to Alzheimer’s,” she explained.
“We’re woefully under-hydrated. If somebody has brain fog,
I’ll have them drink at least half their body’s weight in ounces of water …
Something as simple as making sure you get the appropriate amount of
water can improve your mental and physical state.”
Willeumier’s published research, Reversing Brain Damage in Former NFL Players illuminated just how powerful nutrient support can be when used consistently over time. The study followed 30 retired NFL players who demonstrated brain damage and cognitive impairment. The protocol included fish oil, a high-potency multiple vitamin, a formulated brain enhancement supplement like acetyl-l-carnitine and an antioxidant activity like alpha-lipoic acid or n-acetyl-cysteine.
After six months of treatment, the Microcog Assessment of Cognitive Functioning, a screening tool for brain health, showed “statistically significant increases in scores of attention, memory, reasoning, information processing speed and accuracy.” Most impressive was their brain SPECT scans, which collectively showed increased blood flow to the brain, which ultimately supports mood and memory.
Last but not least, Willeumier said chronic dehydration is linked to many different disorders. “We’re woefully under-hydrated. If somebody has brain fog, I’ll have them drink at least half their body’s weight in ounces of water. The Institute of Medicine actually recommends drinking 3.7 liters of fluid per day for men and 2.7 liters of fluid per day for women. Something as simple as making sure you get the appropriate amount of water can improve your mental and physical state.”
According to Fotuhi, whether you have brain fog from the coronavirus, the stress of a pandemic, or simply want to take steps to prevent it, being proactive with treatment is key: “People need to treat brain fog as they would a urinary tract infection or a rash.” he said. “If you have a skin rash, you don’t just sit there and look at it. You have to do something about it.”
Contact Genevieve Glass at genevieve@beingpatient.com