Viagra may also reduce the risk of developing Alzheimer’s or dementia. While this link isn’t causative, the new research opens the door for clinical trials into efficacy.
Believe it or not, Pfizer’s drug Viagra was originally designed to treat cardiovascular problems. Early on in clinical trials, men taking the drug became nervous when nurses came into the room to check in on them. It became obvious that the drug was successful at increasing blood flow, though not where Pfizer intended. Thus, the story goes, researchers accidentally discovered that the active ingredient in Viagra, sildenafil, treats erectile dysfunction.
In an act of further serendipity, researchers have now discovered that Viagra is associated with a lower risk of developing Alzheimer’s or dementia. A recent study published in the journal Neurology found that men who were prescribed Viagra had an 18 percent lower risk of developing Alzheimer’s. Men prescribed the drug more often had an even lower risk of developing dementia.
These findings aren’t as eye-popping as another study from 2021, which according to headlines from the New York Post, “Taking Viagra cuts the risk of Alzheimer’s by up to 69 percent.” Meanwhile, The Guardian proclaims: “Viagra could be used to treat Alzheimer’s disease, study finds.” Both of these headlines, however, are inflating and misrepresenting the new study’s findings.
This study looked at electronic health data from 269,725 men over the course of 5 years. Half were prescribed Viagra or similar drugs to treat their erectile dysfunction while the other half went untreated. The men who received Viagra were less likely to develop Alzheimer’s disease but that doesn’t mean Viagra prevents Alzheimer’s. The authors of the study themselves concluded that more research is needed, which will include women who are more likely to develop Alzheimer’s than men, to confirm that these drugs indeed reduce the risk of Alzheimer’s.
What about previous findings?
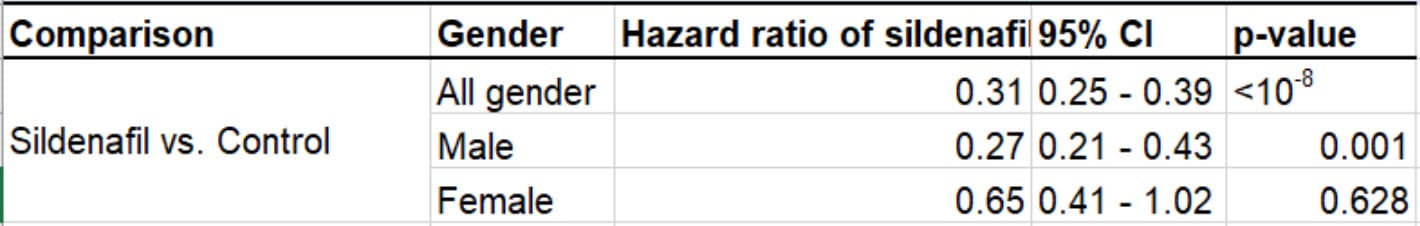
In research published in Nature Aging in 2021, scientists investigated a dataset of 7.23 million individuals through data obtained from insurance claims. When controlling for age, sex, race, and disease comorbidities, the scientific team at the Cleveland Clinic’s Genomic Medicine Institute found that Viagra was associated with a 69-percent reduction in Alzheimer’s risk after a six-year follow-up.
People taking Viagra also showed a significant reduction in Alzheimer’s risk compared to people taking common blood-pressure-lowering or diabetes medications like losartan, metformin, diltiazem, and glimepiride.
However, when the data were stratified by sex, the reduction was only significant in males (see Supplementary Table 9) who are both more likely to be prescribed Viagra, and less likely to develop Alzheimer’s. This means that the majority of this risk reduction comes from the effect in males, while the results did not find a significant reduction in the risk for females who took Viagra, despite that females have a higher likelihood of developing dementia than males.
“Notably, we found that sildenafil use reduced the likelihood of Alzheimer’s in individuals with coronary artery disease, hypertension, and type 2 diabetes, all of which are comorbidities significantly associated with risk of the disease, as well as in those without,” Cleveland Clinic computational biologist Feixiong Cheng, a senior author of the study, said in a news release.
To identify Viagra, the researchers used a computational approach to look for drugs with the potential to impact pathways implicated in Alzheimer’s.
“We hypothesized that drugs targeting the molecular network intersection of amyloid and tau endophenotypes should have the greatest potential for success,” Cheng said, adding that Viagra also improved cognition and memory in animal models of Alzheimer’s disease.
Cheng’s group also tested the effects of sildenafil on cells in a dish to see whether it could reduce tau, a toxic protein that aggregates in tangles in brains with Alzheimer’s. However, Jack Auty, lecturer in the Medical Sciences at the University of Tasmania, noted in a reaction to the study that the drug was administered to these cells at a very high concentration, “around 100 times that achieved by taking the pill.”
Could Viagra treat Alzheimer’s?
Earlier this year, a class of blood pressure medications and a water-retention drug were found to reduce the risk of cognitive decline or Alzheimer’s. Viagra isn’t the first blood pressure drug associated with risk-reduction in Alzheimer’s. But that doesn’t mean it’s reducing people’s Alzheimer’s risk. While studies with large datasets are able to find these strong links between Viagra use and lower risk, the studies haven’t proven any kind of cause-and-effect relationship between the two things — and there are plenty of other variables at play. The authors of the 2021 study, along with other neuroscience researchers, point to limitations in the research that prevents them from claiming sildenafil could be a preventative agent against Alzheimer’s.
“There are other possible explanations for these findings; for example, we know that brain changes start decades before dementia symptoms, and it is possible that these early Alzheimer’s changes reduce sex drive (thus people wouldn’t ask for a prescription for erectile dysfunction),” Tara Spires-Jones, deputy director of the centre for discovery brain sciences, University of Edinburgh, wrote of the 2021 study.
Because the 2021 study’s findings only establish an association between sildenafil use and reduced incidence of Alzheimer’s disease, rather than a proven link, Cheng said, his team is now planning a mechanistic trial and a phase II randomized clinical trial of sildenafil, in order to test causality and confirm the drug’s clinical benefits for Alzheimer’s patients.
UPDATE February 21, 2024, 10:07 P.M. – This 2021 article was updated with new context in light of a 2024 study.