Image: Aduhelm, Biogen/AP.
“The approach I’ve been taking is that each decision about whether or not to offer this as a treatment has to be made on a case-by-case basis.”
UPDATE: 3 March 2024, 8:28 P.M. ET. In February 2024, Biogen took Aduhelm off the market, citing financial concerns. Although the drug did receive accelerated, conditional FDA approval for the treatment of early Alzheimer’s disease in 2021, it is no longer available to new patients. The company announced it would sunset trials in May 2024 and cease supplying the drug to current patients in November 2024.
This month, a flurry of inquiries began landing in doctors’ mailboxes and over the phone: What do you think of Aduhelm? How much does it cost? Is this the right treatment for me or my loved one?
At the Banner Alzheimer’s Institute, dozens of daily calls poured in on the week of June 7 as patients and their loved ones sought after answers about Aduhelm (aducanumab), the first Alzheimer’s drug to be FDA-approved in nearly 20 years.
Because “we had so many calls in the first week, we actually had to dedicate somebody to answering those questions by phone,” Dr. Pierre Tariot, director of the Banner Alzheimer’s Institute, told Being Patient of inquires about the new drug. “We couldn’t just use our normal phone coverage.”
He added, “We have questions coming from either family, or patients themselves ranging from those with very minimal symptoms to no symptoms [and] at risk [of Alzheimer’s], to very severe disease including nursing home residents. The number one question is: ‘Can I get this for me or my family member?’”
The approval of the first disease-modifying therapy for Alzheimer’s has spurred excitement among patients and their families. Up until June 7, the day when Aduhelm received the FDA’s green light, available medications could only treat symptoms of Alzheimer’s without addressing the underlying disease. Aduhelm, on the other hand, targets amyloid plaques that are found in the brains of people with Alzheimer’s, aiming to slow the progression of the disease.
However, the FDA’s decision has garnered no small amount of controversy. The approval went against the objections of the FDA’s independent advisory committee, which overwhelmingly rejected evidence of the drug’s efficacy last November. Some experts have criticized the agency for raising false hope within the Alzheimer’s community, approving a drug despite little evidence of its benefits.
Given the questions and debates about the FDA’s decision, navigating the ins and outs of Aduhelm, such as its eligibility, efficacy, safety and cost can be all the more confusing. Being Patient spoke with clinicians about the common questions regarding Aduhelm, and what we know and don’t know about the treatment so far.
“Clearing amyloid does not cure the disease, so this is by no means a cure.
The disease still [progresses]. But the question now is whether it decreases
that rate of progression to a significant degree, and whether
the magnitude of change justifies the known risks.”
On eligibility, insurance and cost
While the FDA approved Aduhelm for all patients with Alzheimer’s, the drug has only been tested on those in the earliest stages of the disease, and insurers are expected to be key players in shaping patients’ eligibility for treatment.
“The FDA indication is [an] extremely broad treatment of Alzheimer’s disease,” Tariot said. “But the studies didn’t look across the full spectrum of Alzheimer’s disease … and it appears as if payers are going to be the ones most likely to influence who is eligible.
“We expect there to be some regional variation in eligibility and availability. We expect different insurance products to have different approaches.”
Currently, private insurers and Medicare are still figuring out their plans for Aduhelm, which costs $56,000 annually per patient. Adding to that bill are imaging, physician and infusion center expenses.
For Cigna, the insurer’s Chief Clinical Officer Dr. Steve Miller told the Wall Street Journal that it would likely cover Aduhelm for those with early-stage Alzheimer’s and elevated levels of amyloid plaques, matching the profile of participants in Aduhelm’s clinical trials. However, he said out-of-pocket costs for testing could be a major challenge for those who lack financial resources.
Biogen and Eisai, Aduhelm’s developers, estimate that 40 percent of patients eligible for the drug (as determined by clinical trial criteria) will have an out-of-pocket cost of roughly $200 or less annually, and half of eligible patients will have a cap on out-of-pocket expenses.
For the estimated 10 percent of eligible patients without supplemental Medicare coverage, Biogen and Eisai project that they could still be on the hook for about 20 percent of out-of-pocket costs, which could be upwards of $10,000 per year.
It remains unclear exactly how Medicare would handle Aduhelm’s coverage, and the Centers for Medicare & Medicaid Services is planning to offer additional information soon. The federal agency is now reviewing the FDA’s decision.
On availability
According to Biogen and Eisai, clinicians can now prescribe Aduhelm for appropriate patients. That said, the American Association of Retired Persons reports that gearing up to administer Aduhelm will likely take some time. Dr. Richard Isaacson, director of the Alzheimer’s Prevention Clinic at Weill Cornell Medicine, told AARP that “there are just lots of logistical and operational concerns to be sorted out. I would expect that over the coming few months, more and more centers will be able to accommodate patients, but it’s going to be a very metered and I would say a step-by-step progression.”
On efficacy
Aduhelm, which is administered via intravenous infusion, has proven to be effective in clearing amyloid plaques. But whether or not patients’ cognitive and functional impairment will improve as a result remains an open question.
The FDA’s accelerated approval was based on Aduhelm’s effect on removing amyloid plaques, which the agency said “is reasonably likely to predict a clinical benefit to patients.” Still, the FDA stated that “there remains some uncertainty about” this benefit, and to verify trial results, it conditioned Adulem’s approval on a new clinical trial of the drug.
Two Phase 3 clinical trials of Aduhelm were halted prematurely, following an analysis showing that the drug was unlikely to benefit patients. Biogen then analyzed additional data, finding that Aduhelm failed to show benefits in one trial, but the drug slightly slowed patients’ decline in another trial.
“The medication (Aduhelm) efficacy is in question because of the discrepancy in the clinical trial results,” Dr. Zaldy Tan, medical director of the Jona Goldrich Center for Alzheimer’s and Memory Disorders, told Being Patient. “If it is in fact effective, the magnitude of change will likely be modest.”
A takeaway from the clinical trials “is that clearing amyloid does not cure the disease, so this is by no means a cure,” Tan said of Aduhelm. “The disease still [progresses]. But the question now is whether it decreases that rate of progression to a significant degree, and whether the magnitude of change justifies the known risks.”
On side effects
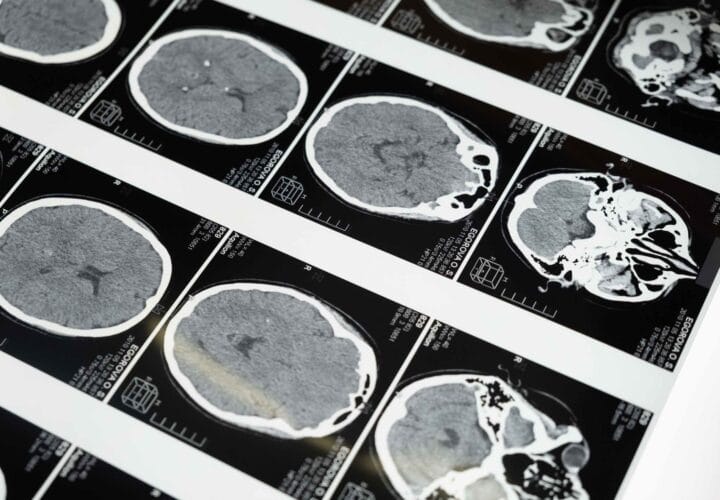
One of Aduhelm’s main side effects is swelling or bleeding in the brain, collectively known as amyloid-related imaging abnormalities (ARIAs).
In the two Phase 3 clinical trials, ARIAs occured in 40 percent of patients receiving the highest dose of Aduhelm, which seems to be the effective dose for slowing decline. Participants who were ApoE4 carriers, the genetic variant that increases Alzheimer’s risk, had greater chances of developing these side effects.
ARIAs were typically asymptomatic, and for patients who did experience symptoms, headaches were the most commonly reported ones. Regular MRIs are therefore needed to monitor for potential ARIAs.
Making an Informed Decision
Before pursuing treatment, Isaacson said there should be thorough discussions between patients, families and clinicians about issues including the risks, costs and scientific evidence of Aduhelm.
As he told AARP, “The approach I’ve been taking is that each decision about whether or not to offer this as a treatment has to be made on a case-by-case basis.”