A recent cell study shows that experimental Parkinson’s and Alzheimer’s antibodies may trigger harmful brain inflammation—which could explain clinical trials’ dismal failure rates.
In the 1990s, drug makers began developing antibodies for treating Alzheimer’s and Parkinson’s — therapies designed to clear aggregates of proteins found in the brains of people with the diseases. But after decades of research, clinical trials of these investigational antibodies showed that the drugs have largely failed to slow patients’ cognitive and functional decline, despite showing initial promise in mice studies.
Scientists have proposed various ideas as to why that’s the case, but a recent study of immune cells derived from human stem cells presents a new explanation, at least in part, for antibody clinical trials’ poor track record: These drugs may carry unintended side effects, reversing any benefits they could provide from removing the accumulation of abnormal proteins. One such unintended side effect is brain inflammation.
The study, published in the Proceedings of the National Academy of Sciences, showed that investigational antibodies for Alzheimer’s and Parkinson’s that target the accumulation of beta-amyloid and alpha-synuclein, respectively, can lead to harmful neuroinflammation. In particular, the scientists found that these investigational drugs triggered an inflammatory response in microglia, the brain’s immune cells, which were derived from human stem cells. This response in turn heightened inflammation, injured neurons, and eventually led to neuronal death.
According to the researchers, this side effect has likely been overlooked in past research, most of which has been limited to mouse studies. But according to Dr. Stuart Lipton, the study’s co-senior author, these findings show that mouse microglia respond differently to antibodies — and that difference in response could account for this unexpected outcome in human-derived microglia.
“In a mouse context, where basically all preclinical work is done, all those antibodies get rid of amyloid or alpha-synuclein and they make the animal in several ways better,” Lipton told Being Patient of antibodies tested in the study. “But if you look at human microglia, unlike mouse microglia, they actually get inflamed much more by the presence of the antibody with its cognate protein. That was a total surprise.”
For the study, the team developed microglia from human stem cells that reflected closely with actual human microglia, and generated much quicker than those from previously reported protocols. Then, the scientists probed the human-derived microglia with misfolded alpha-synuclein, finding that these proteins triggered an inflammatory state in the cells. Furthermore, abnormal beta-amyloid proteins made matters worse.
However, experimental antibodies led to even more inflammation, both in cell cultures and mice models, after successfully hitting their targets. In particular, human-derived microglia that were transplanted to the brains of humanized mice became inflamed, but not mice microglia, Lipton explained.
“It’s pretty clear that human microglia have these very special attributes — they’re exquisitely sensitive to these antibodies,” said Lipton, who is the Step Family Foundation Endowed Chair in the Department of Molecular Medicine at Scripps Research.
Want to learn more about clinical trials
for Alzheimer’s and dementia?
Check out the Lilly Trial Guide.
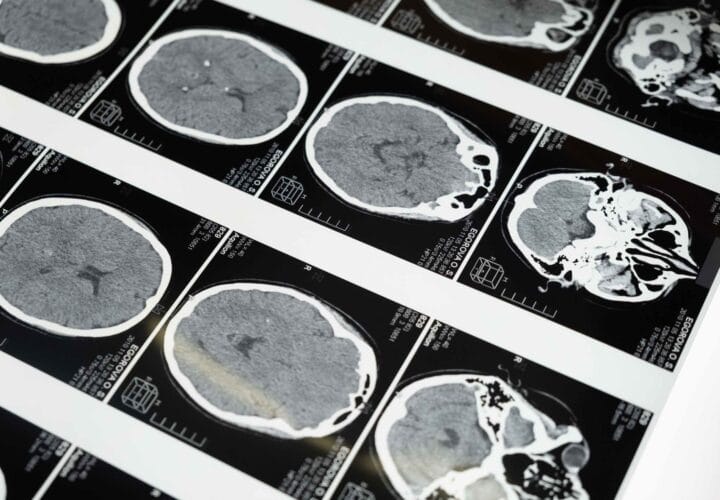
Scientists have known that antibodies can lead to side effects like amyloid-related imaging abnormalities (ARIAs), which are associated with various forms of inflammation. ARIAs, characterized by microbleeds and swelling in the brain, are major side effects reported in clinical trials of drugs including the newly-approved antibody Aduhelm (the drug was not tested in the recent study).
(In February 2024, Biogen took Aduhelm off the market indefinitely.)
But, Lipton believed ARIAs are “the tip of the iceberg.” He noted: “I think there’s potentially many more inflammatory pathways that need to be abated if we’re going to really take advantage of these antibody therapies.”
The good news is that Lipton and colleagues are now developing experimental drugs to counter microglial inflammation triggered by antibodies.
“My hypothesis is that clearing these misfolded proteins that [are] part of the disease potentially is helpful, but it’s also inducing inflammation that’s not helpful,” Lipton said. “I think it would be very interesting to test our new drugs in combination with the antibodies and try to prevent the inflammatory component.”
UPDATE: 3 March 2024, 9:42 P.M. ET. In February 2024, Biogen took Aduhelm off the market, citing financial concerns. Although the drug did receive accelerated, conditional FDA approval for the treatment of early Alzheimer’s disease in 2021, it is no longer available to new patients. The company announced it would sunset trials in May 2024 and cease supplying the drug to current patients in November 2024.

Kindly always provide citations for research articles. thank you.