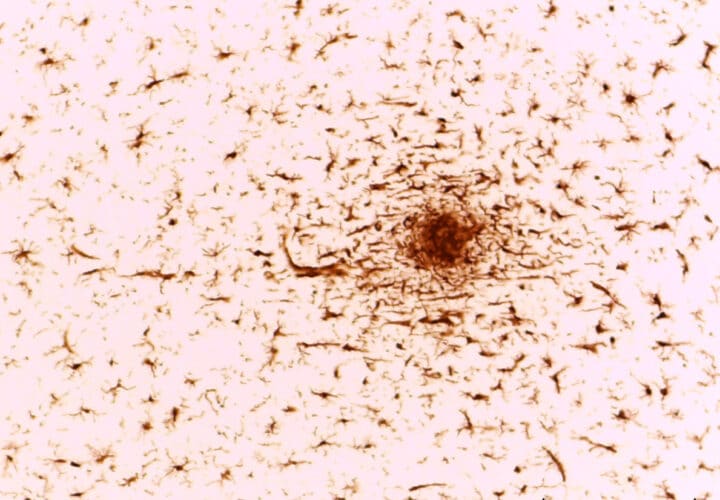
For decades, researchers have been searching for ways to combat the abnormal proteins that appear in the brains of people with Alzheimer’s. Despite their best efforts, the drugs that take aim at the beta-amyloid protein clumps have yielded disappointing results.
But there’s reason for optimism. In the largest Alzheimer’s study to date assessing the networks of more than 3,000 proteins, researchers found that the glucose metabolism of the brain’s support cells could potentially serve as a drug target and biomarker in spinal fluid tests.
“By measuring all these different proteins, you can group them together into different biological processes and pathways,” said Dr. Erik Johnson, a physician-scientist researching neurodegenerative disorders at the Department of Neurology at Emory University in Atlanta. “And that can give you a better, more holistic understanding of what’s changing in the brain during the onset and the progression of the [Alzheimer’s] disease.”
The team analyzed proteins in more than 2,000 postmortem human brains and nearly 400 cerebrospinal fluid samples of people with Alzheimer’s, those who were healthy and those whose cognitive abilities were intact but had documented brain pathology. The researchers classified the proteins into 13 categories, searching for links between the various networks of protein, risks of Alzheimer’s and cognitive impairment.
The study found that the sugar metabolisms of microglia and astrocytes accelerated in the brain samples and cerebrospinal fluid samples of study participants with Alzheimer’s and those who were asymptomatic with the disease.
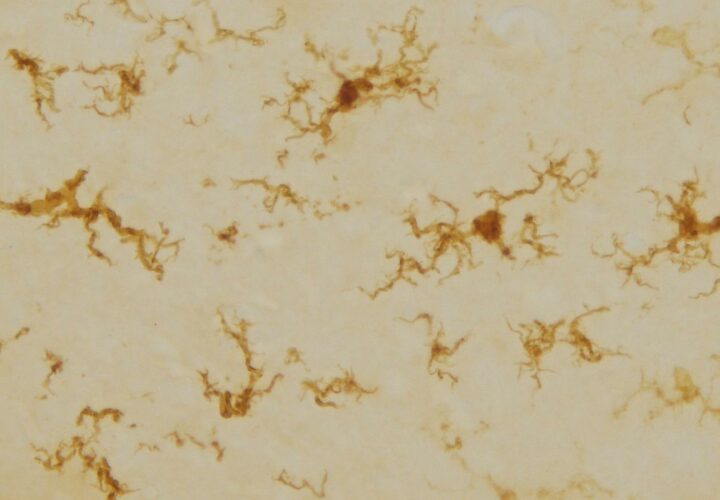
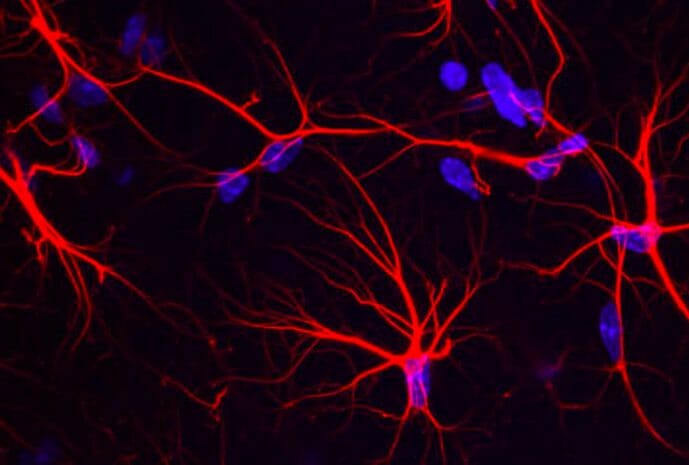
Johnson suggested that to protect the brain, astrocytes and microglia may ramp up their metabolisms as they mount their attack against tangled proteins. Microglia are cells that are critical to brain maintenance—they help seek out plaques, damaged neurons and synapses and infection. Astrocytes, the brain’s most abundant glial cells, regulate transmission of electrical impulses within the brain.
Past studies also found that microglia cells activate in response to amyloid plaques during early stages of Alzheimer’s. Scientists suggest that proteins called TREM-2 maintain the microglia’s metabolic fitness, sustaining their energy to clean the brain’s debris. Prior research shows that lower rates of glycolysis — the process by which the brain breaks down glucose — is linked to more severe plaques and tangles in the brains of people with Alzheimer’s.
That still leaves researchers with the question: Do these heightened levels of metabolism benefit the brain?
After all, microglia can also produce pro-inflammatory proteins. When the cells rev into overdrive, they can damage the brain’s neurons and aggravate inflammation in the brain.
The team found that the microglial cells were associated with anti-inflammatory characteristics. But according to Johnson, more research needs to be done to examine microglia in isolation. Their interpretation should be taken with some caution as it’s difficult to differentiate microglia responses from their mass analysis of proteins. With a better understanding of microglia’s various functions, scientists could potentially develop therapeutic approaches to encourage the cells to produce more beneficial responses, Johnson said.
In future research, the team will use new technologies to analyze at least double the number of proteins, broadening their search for indicators of Alzheimer’s, biomarkers that could pave the way for drugs targeting Alzheimer’s.