Neuroscientist Kristen Willeumier, author of “Biohack Your Brain,” discusses the symptoms of stress-related brain fog and strategies to combat it.
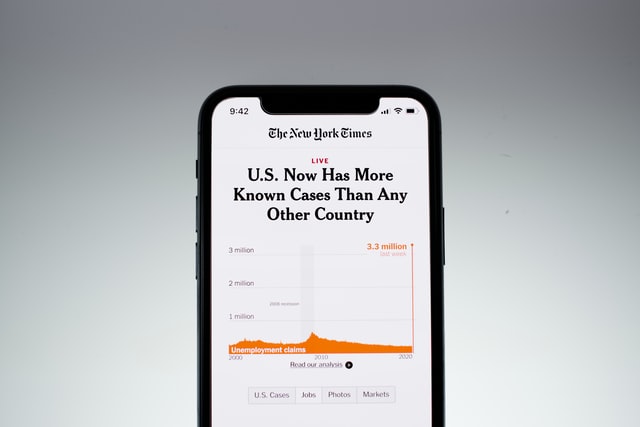
During these unprecedented times, feelings of depression and anxiety are higher than ever as people cope with physical isolation, job loss, anxiety and grief. Difficulty planning, thinking and completing day-to-day tasks efficiently are increasingly common — and cognitive health experts say they could all be related to the stress of the pandemic.
Meanwhile, some people recovering from COVID-19 are experiencing neuropsychiatric symptoms — from insomnia to foggy thinking to depression — that experts say could be associated with the virus.
While ‘brain fog’ can make it harder to function, experts say there are steps people can take in their daily lives to bounce back. Being Patient spoke with neuroscientist Kristen Willeumier about ways to improve brain health and clear the fog.
- Brain fog is a term that describes symptoms such as headache, fatigue, dizziness and the inability to concentrate and remember.
- Maintaining good nutrition and sleep habits, exercising and managing stress are all strategies that can help address brain fog.
- SARS-CoV-2, the virus that causes COVID-19, can trigger systemic inflammation in the body, leading to damages in the nervous system.
Being Patient: What is brain fog?
Kristen Willeumier: Brain fog is a constellation of symptoms. It can be headache, dizziness, inability to concentrate, inability to remember things, malaise or fatigue. For each person, it could be different, but it’s just that inability for your mind to function efficiently.
Being Patient: How common are neurological symptoms in COVID patients?
Kristen Willeumier: The research coming out of China, one of the first big studies, out of 214 people, approximately 30 percent to 36 percent of people had neurological complications. The primary neurological symptoms are loss of smell, loss of taste, headache, brain fog. Certain people are at higher risk for stroke … A smaller percentage of people are having encephalopathies of the peripheral neuropathies, Guillain-Barré [syndrome].
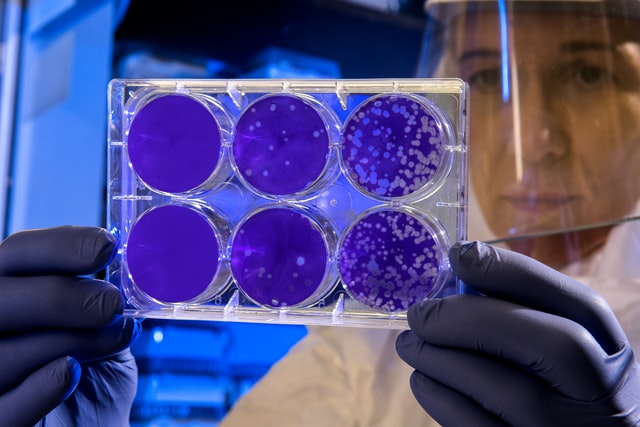
Being Patient: How is the virus able to damage the central nervous system?
Kristen Willeumier: With COVID-19, we’re finding that one of the primary routes of entry into the central nervous system is through the olfactory epithelium, and then it leads back into the nasal passages, olfactory bulb, and can get into the brain.
The other way is you have this systemic inflammation that can degrade the blood-brain barrier, and the virus can potentially get in. The brain fog can be coming from the inflammatory processes that are happening.
Our brain is one of the most metabolically active organs. It weighs 2 percent of our body’s weight and it consumes 20 percent of the brain’s oxygen and energy. When we have this systemic inflammation, the antioxidant systems that are usually there to help protect it are overwhelmed. That’s part of the reason why we can use anti-inflammatory diets to help address some of this brain fog and fatigue that people with COVID are experiencing.
Being Patient: Is inflammation in COVID the same type of inflammation we get from Alzheimer’s or even just a bump in the knee?
Kristen Willeumier: When you bump your knee or get a bruise, you have this acute inflammatory response and it focuses right on that area to help get blood flow and help heal that particular area.
When we’re talking about Alzheimer’s type dementia, you have the accumulation of these beta-amyloid plaques and tau tangles that start decades in the brain before you have a symptom. That’s where the inflammatory response is a little bit different.
With COVID, the difference there is that you have this massive inflammatory response. It’s so overactive and the body can’t handle it. What’s an inflammatory response? There is a release of what are called pro-inflammatory cytokines. They can poke holes in cell membranes and create free radicals that damage the cells and the DNA inside the cells. There’s IL-1 (Interleukin-1), IL-6 (Interleukin-6), tumor necrosis factor alpha. All of these cytokines get released and damage the brain. In COVID, it’s a storm.
Being Patient: Could this kind of inflammation accelerate dementia?
Kristen Willeumier: It absolutely could accelerate the symptoms of people who have dementia because a lot of these diseases of aging are chronic inflammatory diseases. COVID on top of it is like the double hit, which is why we really want to make sure the older populations are protected.
Being Patient: How are clinicians treating the inflammation in COVID patients?
Kristen Willeumier: First, you treat COVID with the antiviral therapies, or some people are using steroids therapies to help and there’s a lot of support from certain nutritional approaches.
Diet is actually one of the smart strategies people can use. Following a Mediterranean diet can actually help improve cardiovascular health and reduce the onset of neurodegenerative decline. So I like people embracing Mediterranean diet, properly hydrating, thinking about the use of smart nutritional supplements.
We’ve all heard vitamin D can be very helpful, or at least making sure your vitamin D levels are managed, because that helps to support your immune system. We’ve got that, we’ve got zinc, we’ve got vitamin C. There are some very basic things that we can all do at home to help protect our brain.
If you have symptoms, like anxiety, and depression, and some of the neuropsychiatric comorbidities, taking things like omega-3 fatty acids can help to manage mood.
Symptoms will eventually resolve. That’s the good news. [It depends] on where somebody is on the spectrum: are they young and were they healthy before they got COVID? [Those people are] going to bounce back a lot quicker than somebody who’s older and has multiple comorbidities. That’s why the older populations are the ones who tend to be more vulnerable and hospitalized. Those are the ones that we see are in our morbidity and mortality statistics.
Being Patient: What can we learn from brain fog and inflammation associated with COVID-19?
Kristen Willeumier: Inflammation in the body leads to pretty much every chronic and degenerative disease: cancer, stroke, Parkinson’s, Alzheimer’s. [COVID-19] is going to make people think more about their dietary and lifestyle habits to help reduce inflammation in the body. Even having excess weight on your body is inflammatory, and can damage the brain. We’ve published research showing that even for healthy individuals that were overweight, having excess weight on the body damages neurons in the brain, especially in the frontal lobes, which is the area of the brain important in higher level cognition and judgment and reasoning.
We’ve got people who are struggling with COVID, the long haulers who have various psychiatric and neurocognitive issues, and it’s getting people wanting to investigate more [about] ‘what do I do? How do I take care of my brain health? Because I don’t want to live like this.’
The interview has been edited for length and clarity.
Contact Nicholas Chan at nicholas@beingpatient.com