A neurologist explains why diagnosing — and telling apart — epilepsy, cognitive decline, and dementia can be so complicated.
As people age, the wear and tear on their blood vessels caused by high blood pressure, cholesterol, or other cardiovascular risk factors, damages the brain and predisposes it to a variety of different diseases including dementia and epilepsy — a disorder characterized by recurrent seizures.
Epilepsy isn’t a rare condition either. In the U.S., it affects roughly three million adults. And as it turns out, epilepsy can make the brain more vulnerable to Alzheimer’s and other forms of dementia. Scientists have found that seizures can cause a build up of beta-amyloid plaques, a hallmark of Alzheimer’s.
This is where things get complicated: While epilepsy may increase the risk of developing dementia, dementia may increase the risk of developing epilepsy by as much as five to 10 times. “The presence of epilepsy in dementia has been shown to be associated with faster cognitive decline and worse outcomes,” Dr. Irfah Zawar, a neurologist and assistant professor at the University of Virginia, Charlottesville told Being Patient. “We found epilepsy to be independently associated with mortality in people with dementia.”
Epilepsy and dementia are also easy to confuse for one another when standing alone: Some types of seizures can cause temporary confusion and memory problems that look like dementia, and that can lead to a misdiagnosis of mild cognitive impairment or dementia in people who only have epilepsy.
Epilepsy can speed up cognitive decline
In December 2023, Zawar presented recent research findings at the American Epilepsy Society Annual Meeting that suggest people with epilepsy who have worse cardiovascular health are at an even higher risk of developing MCI and dementia. The study looked at 13,700 cognitively healthy participants over the course of 14 years, and about 1 percent of these participants had epilepsy.
“We found that people with epilepsy had earlier conversion [to MCI],” she explained. Those with high cholesterol, blood pressure, or diabetes were even more likely to develop the cognitive impairment over a 14-year period. People with active epilepsy were also developing dementia several years earlier than people with epilepsy who were in remission and those who did not have epilepsy in the first place.
However, Zawar and her colleagues didn’t have a lot of information about the type of epilepsy people had, or a lot of details on which anti-seizure medications they were taking. This is especially important data to account for, as — adding to the intertangling of epilepsy and brain health — some anti-seizure medications have been shown to potentially provide a small memory boost.
Epilepsy is sometimes confused for cognitive decline
According to Zawar, some people with a form of epilepsy called temporal lobe epilepsy can be misdiagnosed with dementia.
They experience transient epileptic amnesia which causes up to several minutes of forgetfulness or extreme confusion.
“Patients have [these] episodes often after they wake up where they are completely forgetful,” Zawar said. “They are still able to talk to you, but they can’t recall anything.” They might forget their maiden name, where they are, and even their own date of birth.
The main difference between these epilepsy and dementia is that forgetfulness is very episodic. People who have seizures when they wake up will return to their baseline cognitive function a few minutes later. Meanwhile, people with dementia or other forms of cognitive decline will be impaired throughout the entire day.
“Because these are episodes of forgetfulness, and not necessarily like chewing, or staring off unresponsively, people think this is the onset of dementia,” she added.
Cognitive impairment is a condition that causes memory problems, confusion, and other problems with thinking and planning. It is sometimes caused by Alzheimer’s or another form of dementia, or a slew of other conditions like vitamin deficiencies, metabolic problems, depression, and sleep disorders.
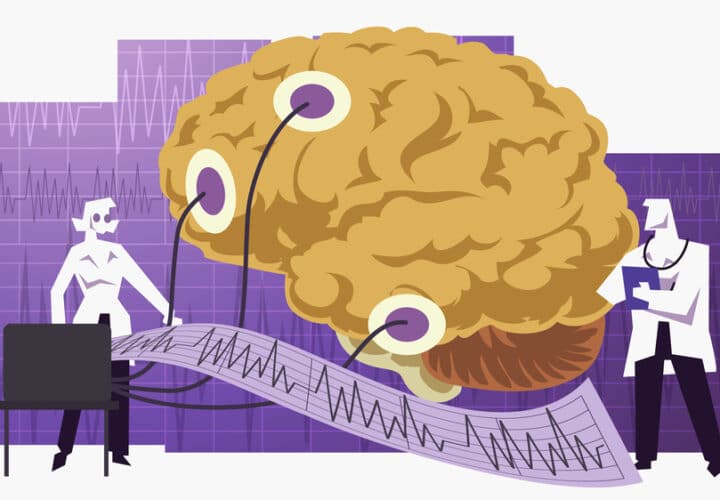
In epilepsy, the brain’s electrical signals start to misfire causing recurrent seizures. If the misfiring occurs in the part of the brain that is involved in memory, it can lead to brief bouts of confusion and memory problems. Unlike cognitive impairment or dementia, these symptoms are temporary.
How do doctors tell the difference between epilepsy and early signs of dementia?
Making sure people receive an accurate diagnosis can ensure their underlying condition, whether it be MCI, dementia, or epilepsy is treated appropriately.
Diagnosing dementia is complicated. It involves cognitive tests to measure the extent of cognitive impairment, blood tests to look for any underlying conditions that could cause cognitive decline. A lumbar puncture or amyloid PET scan is also used to rule out or confirm an Alzheimer’s diagnosis — the most common form of dementia.
Right now, when people go in to get tested for dementia, they seldom receive a test that can detect epilepsy — electroencephalography. An EEG involves sticking a bunch of electrodes onto a person’s head to look for abnormalities in the brain’s electrical signaling. Often, Zawar explained, people will need to get an EEG while they’re sleeping to detect temporal lobe epilepsy.
“We know that the diagnostic delay of epilepsy in people with dementia can be several years because seizures typically present with confusion in people with dementia,” Zawar said. “They already have some subtle ongoing cognitive deficits and confusion and because the seizures are so subtle, they’re so often missed.”
To address these issues, she is researching new strategies and techniques to improve the diagnosis of epilepsy in people with dementia.



I love the articles, they interesting.
I am looking for the article with Dr. Onyike, MD, Johns Hopkins on Early-Onset AD.
I would a copy of the article the
Dr. Onyike of his recent article.
Thank you