Can you improve mild cognitive impairment, or stop its progression? How long does is last? How do you overcome it altogether? Read on to learn from experts what causes this condition — sometimes a precursor to dementia in older adults — and how to treat it.
Feeling fuzzy lately — fuzzier than usual? Some people experience subtle downturns in memory, thinking, and cognition related to age — or to a number of health conditions that can have negative effects on the brain. Doctors might refer to an unexpected decline in cognitive abilities as mild cognitive impairment, or MCI. MCI isn’t a disease unto itself — like the term “dementia,” it’s a set of symptoms, and it can have many underlying causes.
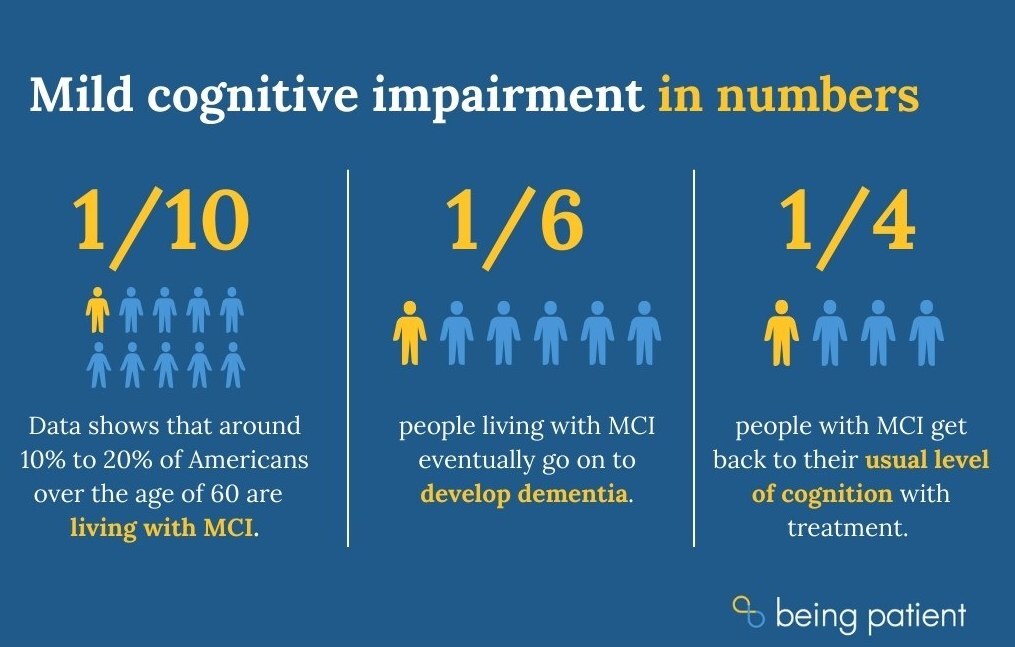
One of these underlying causes is Alzheimer’s, or other forms of dementia. (According to data from a study by the American Academy of Neurology, 10 to 15 percent of patients living with MCI eventually experience a progression to dementia.)
So, while sometimes MCI can sometimes turn into something more serious, the good news is that there are all manner of other underlying causes that can bring about MCI, and many of these causes are treatable. With treatment, one in four individuals do recover from MCI back to their baseline of “normal” cognition. Figuring out and treating the underlying cause or causes of a person’s MCI symptoms may help treat, stop or even reverse it.
What is mild cognitive impairment — and how do I know if I have it?
According to the National Institute on Aging, if you receive a diagnosis from your medical care provider of mild cognitive impairment, it means you’re showing more memory or thinking issues than others your age. This isn’t a diagnosis that’s handed out flippantly. If you’re worried you might have MCI, talk to your care provider, and if they don’t take your concerns seriously, ask for a referral to a neurological specialist.
Neurologists conduct comprehensive neuropsychological evaluations — the gold standard for diagnosing MCI. These might include the Short Test of Mental Status, the Montreal Cognitive Assessment (MoCA) or the Mini Mental State Examination (MMSE).
Symptoms: What does MCI feel like?
According to UCLA’s Sidell-Kagan Alzheimer’s Disease Treatment Development Program Director Sarah Kremen, M.D., those experiencing typical age-related cognitive changes can have difficulty retrieving information from the “rolodex” in their brains.
“This is common when people are trying to name something, either finding a word that they want to use, or frequently even [finding] proper nouns, which would include names of people or famous people,” Kremen told Being Patient in an interview. That “tip-of-the-tongue” moment, when a person can’t seem to find the right word even though they know it’s somewhere in the back of their minds, might grow more frequent for older adults as they age.
If you’re struggling with what’s often referred to as “brain fog” or having other cognitive issues that don’t seem normal to you, MCI might be the cause.
Some forms of MCI only affect memory. This is called amnestic MCI. People might forget previous conversations, or misplace items like wallets and keys. In other cases, MCI affects parts of the brain that aren’t related to memory, causing difficulty with speech or language (also known as aphasia), trouble focusing, and difficulty navigating familiar spaces.
People with MCI often experience things like:
- Frequent forgetfulness
- Losing one’s train of thought
- Getting lost or disoriented in familiar places
- Having a hard time following along with a story or conversation
- Missing appointments or social engagements
- Difficulty with decision-making or judgment
- Difficulty finishing tasks or following directions
MCI can also come with symptoms like uncharacteristic depression, anxiety, aggression or apathy. These same symptoms are also common in people living with Alzheimer’s or another form of dementia — but across the board, MCI’s symptoms are less severe.
If you’re noticing any of these symptoms — or if your friends or family are — it might be time to check in with a doctor. As mentioned, 25 percent of cases of mild cognitive impairment can be reversed with treatment.

So what causes MCI?
Kremen fields a lot of questions along the lines of, “How long does it take to go from mild cognitive impairment to dementia?” But does MCI always lead to Alzheimer’s or other forms of dementia? Older adults can have mild cognitive impairment due to Alzheimer’s, Kremen said, but people also suffer from MCI due to a host of other factors.
“There’s a lot of reasons why people have cognitive impairment,” Kremen said. “You can’t jump to the conclusion that ‘I have mild cognitive impairment, I must have Alzheimer’s disease.’”
If untreated, these other causes could also increase the risk of developing dementia. But treating these conditions may well reverse and clear up MCI. Here are a few of those possible causes.
Sleep issues
People with obstructive sleep apnea, a condition when people’s breath stops for brief periods during sleep, can experience mild cognitive impairment. With proper treatment, clinicians can improve the cognitive abilities of these patients. Some people with insomnia experience MCI. Sleep deprivation and disruptions prevent the brain from resting and recharging. Working with a doctor to improve sleep quality can help reverse this type of MCI.
Hormonal changes
The hormonal shifts occurring during menopause could lead to MCI. Treatment with hormone replacement therapy can reduce many menopause symptoms, including cognitive impairment.
Depression
As many as three in five people diagnosed with depression will experience some form of memory loss or cognitive impairment. Treating the underlying depression with a combination of medications and therapy can alleviate these symptoms.
Metabolism issues
Cardiovascular disease causes the narrowing of arteries, damages blood vessels, and makes it harder to supply nutrients and oxygen to the brain. In this case, lowering blood pressure and cholesterol through exercise, dietary changes, and medications like statins may reverse MCI. Doctors are also exploring the links between cognitive function and hyperthyroidism.
Traumatic brain injury
Traumatic brain injury and stroke damage specific parts of the brain, leading to cognitive and memory problems. In some cases, the cognitive changes can be rehabilitated. However this depends on the severity of the injuries.
Medications can cause cognitive impairment
A review of people’s medication can also provide clues to the cause of older adults’ mild cognitive impairment. For one, Kremen said, medication for treating urinary incontinence can affect their cognition. Over-the-counter sleep medications, or the drug Ativan, commonly used to treat anxiety, may also lead to mild cognitive impairment.
Other health issues can lead to cognitive decline or impairment
Older adults with illnesses such as heart failure, urinary tract infection and thyroid problems can also have the syndrome, Kremen said. Clinicians can improve the cognitive abilities of patients with these conditions with appropriate treatment.
Does mild cognitive impairment automatically mean Alzheimer’s?
“Now on the flip side, if it is [due to] Alzheimer’s disease, then that’s important to know too obviously because that has an impact on the future of your life [and] your family’s life,” Kremen said.
An FDG PET scan, which shows the patterns of metabolism in the brain, can help clinicians paint a better picture of whether the patient has mild cognitive impairment due to Alzheimer’s, Kremen said. Clinicians can also conduct a lumbar puncture, which involves drawing a patient’s cerebrospinal fluid to analyze levels of beta-amyloid and tau, biomarkers of Alzheimer’s. In addition, results from a battery of neurocognitive tests can also help clinicians stitch together pieces of the puzzle. To improve accuracy and accessibility of diagnostics for Alzheimer’s, scientists are developing tools like blood tests and retinal scans.
In general, Kremen said, clinicians in academic institutions have become more aggressive in determining the causes of mild cognitive impairment. That way, if they determine that the syndrome is due to a neurodegenerative disease like Alzheimer’s, they can begin managing people’s symptoms early on, and prepare patients and their families for care planning.
MCI as an early sign of Alzheimer’s disease or other forms of dementia
In the cases where MCI appears as a red flag symptom of Alzheimer’s disease or another form of dementia, cognitive issues are being caused by problematic proteins that clump and tangle which interrupts brain signaling and kills individual brain cells.
The best-known of these proteins are beta-amyloid and tau — two of the key hallmarks of Alzheimer’s disease. After a cognitive screening, a specialist might recommend a PET scan or MRI. If the scans don’t spot these proteins, the doctors can rule out Alzheimer’s disease.
Currently, there is no surefire way to reverse this type of MCI caused by Alzheimer’s disease. Scientists are hoping the new class of drugs that targets beta-amyloid plaques can make the difference. The results of clinical study suggest that Leqembi — which as of July 2023 has full FDA approval — may slightly slow the rate of cognitive decline. The hope is that future drugs will be able to reverse the specific cases of MCI that are caused by Alzheimer’s entirely.
Does this condition away? Science shows some lifestyle changes might stop or reverse MCI
Sometimes, it’s not clear to doctors what’s causing the effects of MCI, but even in this case, there may still be a good chance of reversing it, just by changing one’s lifestyle.
For example, in a 2019 clinical study, medical researchers over the course of four years studied a group of participants with MCI where the cause was unknown. They found that participants who continued to stay intellectually and physically engaged, engaging in activities like driving and using maps, reading books and newspapers, and participating in hobbies and other activities were more likely to experience a reversion to their previous cognitive state and recover from MCI.
What should you do if you think you have MCI?
People who are experiencing symptoms of MCI should confer with a doctor or ask for a referral to a medical professional who specializes in cognitive care — there might be steps they can take to experience a similar reversion and restoration of their memory and other functions.
Dr. Bill Burke, M.D., director of the Stead Family Memory Center at the Banner Alzheimer’s Institute, sat down with Being Patient in 2018 to discuss what patients should ask their medical providers if they believe they or a loved one is having memory issues.
“My goal in going into the doctor is trying to see if there’s something going on that needs to be identified — that there’s something that could be done about it — so reversible causes of cognitive impairment,” Burke told Being Patient. “Generally I would go in and tell my doctor, ‘I’m concerned about my memory.’ They may do a little bit of cognitive screening, which may or may not be helpful. If you’re really anxious, sometimes you don’t do very well on those tests, so they can be kind of tricky.”
As a doctor himself, Burke says, he is concerned with factors that could drive MCI, like depression and anxiety. thyroid function, and vitamin B 12 levels, as well as general blood chemistry and blood count. “Then, he said, “I want to do a neurologic exam to see if there’s any signs of something affecting the brain that we can see a signal of. So has there been a stroke? Might there be a tumor in the brain? So you can do a lot, just strictly with a pretty straightforward physical exam, some really basic laboratory testing, some really basic paper-and-pencil testing, and sort out whether there’s something serious going on or not.”
Can you stop, reverse or cure cognitive decline or cognitive impairment?
According to Kremen, there’s currently no approved medication for mild cognitive impairment, and exactly how long it takes for the MCI caused by neurodegenerative disease — the progressive death of nerve cells in the brain — to bring about dementia symptoms varies from one patient to another. This said, intensive study into this topic shows there are ways to protect and preserve your brain function and in some cases, slow down the progression of MCI or even reverse it, depending on its cause (sometimes MCI can be caused by hormonal imbalances, stress or other treatable factors).
There’s no way presently to reverse MCI caused by Alzheimer’s, but Kremen recommends her patients with mild cognitive impairment due to Alzheimer’s should exercise for 30 minutes a day, whether that is a workout or just an easy walk. Data shows sticking to a healthy sleep routine and managing mental health is also important. Based on research, Kremen also advises her patients to eat a healthy diet that is low in saturated fat, consisting of fish with fatty acid like salmon, along with food with antioxidants like blueberries and cranberries.
What’s the difference between MCI and Alzheimer’s or other dementias?
With aging comes concern about developing Alzheimer’s disease or other forms of dementia, and every lapse in memory or attention can feel like the first sign. However, symptoms of early stage dementia are often similar to many other conditions — including natural aging.
According to Dr. Stephanie Collier, a psychiatrist in the Geriatric Psychiatry Outpatient Services at McLean Hospital, it is important to consider all possibilities.
- Lapses in memory and trouble with focus can be natural signs of aging, not dementia.
- Because of similarities in symptoms between dementia and other conditions, many psychiatrists hesitate to diagnose dementia in early stages.
- People with dementia have a high chance of developing depression and anxiety, which can make cognitive testing difficult.
Collier covers the symptoms of early stage dementia and why diagnosis can be difficult at those stages. Watch that conversation or read the transcript here.
OK, then, how can you tell if MCI and normal aging?
According to UCLA’s Sidell-Kagan Alzheimer’s Disease Treatment Development Program Director Dr. Sarah Kremen, people experiencing typical age-related cognitive changes can have difficulty retrieving information from the “rolodex” in their brains.
“This is common when people are trying to name something, either finding a word that they want to use, or frequently even [finding] proper nouns, which would include names of people or famous people,” Kremen told Being Patient in an interview.
That “tip-of-the-tongue” moment, when a person can’t seem to find the right word even though they know it’s somewhere in the back of their minds, might grow more frequent for older adults as they age. After all, it takes longer for the aging brain to sort through information in the rolodex. With these “normal aging” memory lapses, the person will remember the words they were searching for eventually.
In the case of healthy aging, despite occasional forgetfulness, older adults will still form new memories, Kremen said. “They can remember what they did yesterday. They remember details of something they’ve read or conversations they’ve had. They can keep to their schedules. They can remember doctor’s appointments. They remember how to get to places.”
When these things stop being the case, however, it may be time for a closer look.
What about early-onset Alzheimer’s?
A rarer version of the disease known as early onset Alzheimer’s (which is also known as younger onset) may make itself known at a much younger age. It is estimated to affect between 220,000 and 640,000 Americans. In people with early onset Alzheimer’s disease, symptoms typically emerge between the ages of 45 and 64.
For those concerned about the possibility of developing early onset, experts advise using the old standby of, “If you see something, say something.” If you see something amiss with your loved ones, experts recommend talking to a doctor, and considering cognitive testing. Because many doctors aren’t specially trained to spot early signs of Alzheimer’s, be persistent with your concerns.
Some of the main symptoms to look out for include forgetfulness and memory loss; language impairment; a loss of attention span; personality changes, mood swings, and social withdrawal. Learn more about those symptoms here and if you spot a few of them at once, talk to a doctor about getting cognitive testing.
Additional reporting by Nicholas Chan and Alexandra Marvar



I’ve diagnosed with primary progressive apraxia that affects my speech. Is this a form of dementia ?
What an excellent and encouraging article on MCI. One of the best I have read.
I have friends that are on RA (rheumatoid arthritis) drugs and are suffering profound memory issues. Watching TV and TV News seems to greatly irritate and frustrate them to the point their families limit their TV time.
I have been diagnosed with memory loss due to exposure to loud noise causin tinnitus and memory loss. I take thee meds. Diclofinic, Memitine and other meds to control blood pressure cholesterol. What else can I do. I live a normal life. Am retired with a wonderful wife. What else can I Do?