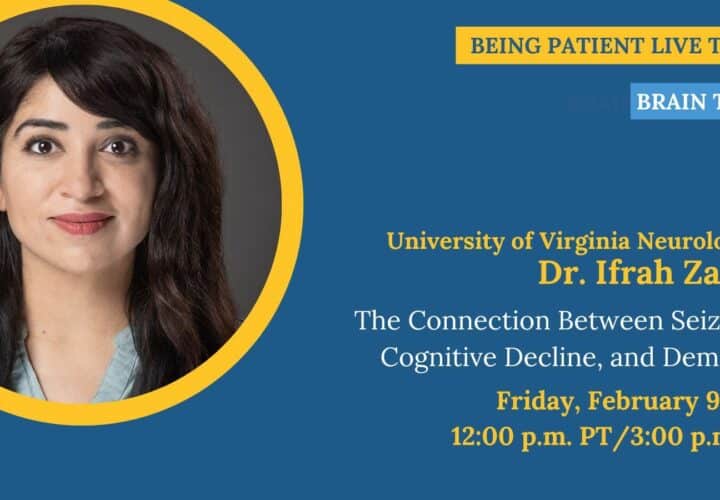
Seizures, cognitive decline, and dementia are linked. Neurologist Dr. Ifrah Zawar joins Being Patient Live Talks to explain the relationship and what people with dementia need to know about epilepsy.
People living with Alzheimer’s disease also live with a higher risk of seizures. And that can make things complicated for doctors: Seizures are sometimes misdiagnosed as cognitive decline — and vice versa.
Complicating this relationship further: Epilepsy, a disorder involving recurrent seizures, can not only mimic cognitive decline — it can eventually lead to it. And cognitive decline, if it isn’t reversed, can give way to dementia.
Seizures, cognitive decline, and dementia — they’re all tangled up together, and it can feel like a chicken-and-egg scenario for diagnosing physicians. Are a patient’s seizures causing their cognitive decline? Or is cognitive decline causing seizures?
Neurologist and epileptologist Dr. Ifrah Zawar at the University of Virginia helps explain the relationship: “The more severe the dementia, the more likely they are to have seizures,” Zawar said. “On the flip side, just like you said, people with seizures also, especially with uncontrolled seizures, often experience cognitive impairment and cognitive decline.”
Zawar serves on editorial boards of epilepsy and Alzheimer’s disease journals and has won multiple awards and recognition for her research. She joined Being Patient founder Deborah Kan in conversation about the link between seizures, cognitive decline, and dementia — and about her clinical and research on seizures and epilepsy in older adults, and epilepsy in people with dementia.
Read or watch the full conversation below and learn more about how seizures can manifest as dementia symptoms, about the similarities between cognitive decline and seizures, and about the extent to which treatments for seizures work with people living with Alzheimer’s disease.
Being Patient: I’ve heard it both ways. I’ve heard of people who have been diagnosed with dementia experiencing seizures, and I’ve heard of people who have epilepsy or seizures, who also experienced cognitive decline. Chicken and egg scenario, as they’re both related. What is the relationship between seizures and cognitive decline?
Dr. Ifrah Zawar: Exactly as you’ve heard, it is the chicken or the egg paradox when it comes to seizures and dementia. It’s a bi-directional relationship. People with dementia are at a higher risk of developing seizures. There are multiple mechanisms underlying why that might be because dementia involves neuropathological changes in the brain, ongoing injury in the brain, or possible inflammation in the brain. All of those can predispose patients to seizures.
The more severe the dementia, the more likely they are to have seizures. On the flip side, just like you said, people with seizures also, especially with uncontrolled seizures, often experience cognitive impairment and cognitive decline. The vast majority of our patients do have at least some degree of mild cognitive impairment. As they continue to age, they can even develop dementia.
So, it is a bi-directional association. The reason why seizures are often associated with cognitive decline is because, obviously, it’s kind of like an electric circuit that’s going haywire, and it’s firing off erratically when it’s not supposed to. Often, it can involve the memory portions of the brain. Over time, once the memory circuits continue to become involved with seniors, that can contribute to memory decline, cognitive decline, and cognitive impairment.
Being Patient: Do we know what causes seizures, or epilepsy for that matter? Actually, let’s define epilepsy. Is epilepsy a specific disease, or does that refer to repeated seizures?
Zawar: Epilepsy basically is defined as recurrent seizures. So, two or more seizures, which are more than 24 hours apart, are defined as epilepsy. Our patients who have a single seizure per day have a 60 percent or higher risk of seizure recurrence. They also are categorized as epilepsy.
Then, there are certain epilepsy syndromes that we know of that present with a certain set of symptoms together. If patients have one of those, then again, they are categorized as epilepsy. So, epilepsy, like you said, is basically recurrent seizures, but they don’t necessarily need to have recurrent seizures. Sometimes, just having a single seizure and [an] increased risk of recurrence can also qualify for the diagnosis of epilepsy, and that means that the patients require treatment in those situations.
Being Patient: Do we know what underlying cause actually contributes to seizures?
Zawar: Seizures can happen from a multitude of different causes. Some patients may have structural abnormalities that can be visible on the MRI. Sometimes [it’s] childhood strokes, tumors, anything that can impact the brain really, trauma, traumatic brain injury, motor vehicle accident, or something that can impact your brain. Anything that can impact the brain can cause seizures.
Like a stroke, tumor, or cancer that spread to the brain or started in the brain, or like traumatic brain injury that resulted in damage to the brain are three examples that I can give, but there are a multitude of other things. For example, in childhood, especially if there is a birth trauma, then the patients may have [a] higher risk of seizures later on in life. Sometimes, malformation of cortical development; that is just the way that the brain forms during the nine months in utero, can also lead to seizures later on in life.
There are some genetic predispositions that can lead to seizures, but they don’t always have to be genetic as well. So, there are a multitude of reasons why seizures may occur, and dementia is just one of them. In older people, dementia, again, is like a progressive disease that will impact the brain and, therefore can also cause seizures.
Being Patient: What part of the brain do seizures involve?
Zawar: They can really involve any part of the brain, depending on where the injury is or where the malformation of cortical development is. Often, one of the more commonly involved regions is the hippocampus or the memory portions of the brain. They tend to be involved pretty commonly, especially in older adults— it’s just the kind of epilepsy that they develop.
Temporal lobe epilepsy [is] the most common type of epilepsy in older adults. But like I said, it doesn’t have to be; it really depends on the region that’s impacted by either a stroke or a trauma or a tumor that the seizures can develop from that region.
Being Patient: I’m just thinking about the chicken and egg scenario. Obviously, we know that Alzheimer’s impacts the hippocampus first. So, I could understand why that would be complex, especially in regard to dementia. What’s the cause or effect, right? We know the biomarkers of Alzheimer’s are beta-amyloid plaque. tangles, inflammation. I heard you mentioned inflammation previously. Do we know if any of those markers actually have an impact in specifically increasing seizure risk?
Zawar: That’s a wonderful question. In the world of clinical research, that question is still unanswered, but there are some animal studies from rats and mice that have shown that inflammatory markers, lower amyloid, increased tau, the kind of pathology that you see in Alzheimer’s disease, can predispose animals to a higher risk of seizures. So, that has been shown— just not in clinical studies.
It’s just something that we are now beginning to study more and more. Typically, epilepsy or seizures are diagnosed with an MRI and an EEG. We typically don’t use a whole lot of other markers. If we suspect a genetic underlying predisposition, sometimes we may do genetic testing for seizures. But you’re absolutely right, especially in the context of dementia and seizures and seizures and dementia, it’s becoming increasingly important to understand how these biomarkers, which are biomarkers of dementia, may impact seizure occurrence.
Being Patient: Do we know what percentage of people diagnosed with dementia have seizures?
Zawar: Up to 64 percent of people with dementia may have seizures, [whereas] studies will show numbers ranging interestingly from point five to 64 percent. But seizures are extensively underdiagnosed in people with dementia.
Being Patient: We have a question from our audience. She’s asking, can we assume that if someone’s dementia symptoms have a sharp increase, there could be undetectable seizures? Could an undetectable seizure cause temporary dementia-like symptoms like global amnesia episodes?
Zawar: Yes, that is an excellent question. Like I said, seizures often are underdiagnosed in people with dementia. When I’m talking to my patients, what I ask them is to look for things which are episodic in nature because that’s the nature of seizures, right? The reason why seizures are under-recognized in people with dementia [is] because dementia patients have ongoing cognitive decline. They have ongoing confusion. They have ongoing memory deficits.
Often when they have episodes of worsening memory deficits when they have episodes of staring, [or] when they have episodes during which they’re confused, their families or even their care providers, even their physicians, may dismiss this as just an episodic worsening of dementia — but those can definitely be seizures.
The way seizures present in younger people and the way they’re present in older people tend to be different. So, older people, especially those with dementia, can have bigger convulsive seizures as well, but they don’t need to. The seizures tend to be very subtle. They’re often very episodic episodes of staring during which the patient may not respond for like five, ten seconds, episodes of confusion, which may be worse than their baseline dementia, and exactly like she said.
So, the term that we use is called transient epileptic amnesia. It basically is a type of temporal lobe epilepsy that will present in older people. Just as the name implies, it’s [going] to have transient episodes or which are epileptic in nature. They are seizures, but they present with mild or like complete memory loss for like five, ten minutes; often, patients will wake up from sleep, and they will have no memory of anything for like a few minutes, and then they will regain that memory.
These patients often may not even have underlying dementia. They will get diagnosed as dementia when they’re just having episodes of transient memory impairment, which are truly just seizures. Then, even in people who have dementia, they can have, just like she asked, transient worsening of memory, transient confusion, just some staring episodes — but anything that is transient or episodic should always raise concern for the possibility of seizures, especially in older people and those with dementia.
Being Patient: My next question is, how do you diagnose this if it’s not an apparent seizure? Staring episodes can also happen without seizures, right?
Zawar: Yeah, but if there are enough risk factors. I would say diagnosis can be a huge challenge, just like you said. If you know of someone [who] is having staring episodes, during which they are clearly not responsive, it’s not that they’re just lost in their thoughts but clearly not responsive, it would be [a] time [to] discuss that with your neurologist— or if you don’t have a neurologist, then you should be seeking a neurologist.
There are sub-specialized neurologists. For example, like me, I’m a neurologist, but I have further training in EEG and epilepsy. But even general neurologists, with a good history, should be able to at least suspect the possibility of epilepsy and then they often pursue the workup that is required for seizures and the diagnosis of epilepsy.
I will also go on to say if I suspect somebody to be having episodes that are concerning enough, because again, since they are episodic, we may not record them on the EEG, I may not be able to see them— if the suspicion is high enough, I would err on the side of starting patients on seizure medications. But for the patients, the next step is to at least seek a neurologist to provide the extensive history that they have and things that they have noticed to get their opinion and at least get the appropriate workup.
Being Patient: We’re getting lots of great questions, so I want to get to them. One is, does inflammation of the lining of our brain cause seizures? Can it cause seizures?
Zawar: Yes, so inflammation of the lining of the brain is really meningitis or the infection of the lining of the brain. Either they can increase the risk of seizures, but there are many patients who have had inflammation or meningitis who may not ever develop seizures— but yes, they can increase the risk of seizures.
Being Patient: Another audience member is asking, are very frequent myoclonic jerks an indication? Those are the jerks you sometimes get in sleep, right?
Zawar: When that jerk happens in sleep, like a lot in sleep, it’s typically what we call a hypnic jerk or a sleep myoclonus. It’s typically a benign thing that happens during the sleep-wake transition. Nothing worrisome. But, if it’s excessive, it’s definitely worth pointing out to the physician. If it happens during the daytime, then they should definitely consider the possibility of seizures and epilepsy and reach out to a neurologist.
Being Patient: Someone else is asking how this differs from TIAs, especially in vascular dementia. Also, could you explain TIA’s for members of our audience that don’t know?
Zawar: TIAs are transient ischemic attacks. So, they are kind of like a smaller sibling stroke, where stroke will present with certain deficits like speech impairment or weakness of part of the body, which may result in permanent deficits because of permanent damage of the brain. Transient ischemic attacks, on the other hand, as the name implies, are transient in nature, so they are just episodes during which the patient may have certain symptoms.
[The] underlying pathology is different because transient ischemic attacks typically happen because there may be [a] lack of blood flow to the brain for a small period of time resulting in that episode. But often, when patients do present with transient ischemic attacks, we do entertain the possibility of epilepsy as well.
The neurologist will do their exam and get their history to tease out whether this seems more consistent with transient ischemic attack, which means the blood flow was temporarily compromised to the brain for some reason, resulting in some certain weakness or speech impairment or certain deficits that went away versus the possibility of seizures.
Altered awareness, I think [is] definitely [the] hard distinction between TIAs and seizure-like episodes, something that perhaps is best made by a neurologist, but I would say if they are otherwise intact, or they are just staring blankly, or have [profoundly] altered awareness, during that episode, I would perhaps be a little bit more inclined to think that these are seizures rather than TIAs.
Being Patient: We have another question. In a case where EEG does not capture the seizures, but they continue occasionally, what are the benefits and/or risks of medication?
Zawar: Unless we do a long-term EEG in which we keep the patient in the hospital, which we do sometimes if needed, we are often not able to record the episodes. Because if somebody has [a] once-a-week seizure, unless we keep them in the hospital for a week, or like send them with a long term, EEG will not be able to record seizures.
Like I said, if we suspect the seizures [and] the chance of seizures is high enough, we do discuss the trial of medications, especially [if the] episodes are happening repeatedly. If their risk [is] otherwise high, like somebody who has a history of stroke or something on the MRI, then it’s more likely that they are truly seizures. Then, we also have to watch for the response to medications, right?
So, if they have like two seizures a week and then some episodes, we didn’t record on the EEG, we started the medication, the episodes improved significantly, that’s another way that’s implying that they were probably seizures. But coming back to the benefits or risks, they vary from medication to medication. Not all medications have the same side effect profile.
It is really a discussion between the patient and the physician and the decision if they’re okay to tolerate the side effects of the medication or not. I would say this: if the patient does truly have epilepsy, and it’s highly suspected by neurologists, then epilepsy is a risk factor for death. With a phenomenon, which is called sudden unexpected death in epilepsy, it is one in one thousand, but it can happen.
So, we tend to, and again, like I said, it will depend on the discussion between the patient and the physician. Often, if the medications are causing side effects, we may switch them to a different medication, which [is] more tolerable to the patient. But because of the risks associated with uncontrolled seizures, it can be so much higher, we prefer for the patients to be on medications.
Being Patient: We have a question that was sent in. This person was diagnosed with benign myoclonus around 1990 and Lewy body dementia in March of 2023. He’s wondering if there are any known correlations?
Zawar: I don’t. As you may be aware, we don’t do anything about it unless it’s significantly bothersome.
Being Patient: What is that exactly? So that people know.
Zawar: They may have subtle jerks, which are not found to have any EEG correlation. Like I said, sometimes they can happen in sleep. If they’re not bothersome, we typically tend not to treat them. So, I am not aware of a correlation between benign epilepsy and Lewy body. If there are some studies out there that I may not have read, I don’t know about them.
Being Patient: I have a question about treatment. Now you’re talking about medications you were referring to drug medications. Personally, I have read studies about epilepsy and the ketogenic diet. I’ve read scientific reports that say that actually, ketogenic diets have been quite successful in controlling epilepsy. What’s the connection there? Is that a viable treatment for people who might be seeking one?
Zawar: [The] ketogenic diet is an FDA-approved treatment for epilepsy. We often use [it] in kids, the pediatric population, with epilepsy, because you know, they will not object to [it] if you feed them a ketogenic diet because the ketogenic diet that we typically use for epilepsy is a very extreme version. The thought is that the presence of glucose in the brain can increase the risk of seizures, which is reduced if the predominant substance ketones are there, then that risk is reduced.
So, the ketogenic diet is certainly an improved treatment for people with certain kinds of epilepsy. It’s the first-line treatment, but for other types of epilepsy, it’s something that we may try after a few medications if the patient is open to it. Most adult patients do not want to and are not able to tolerate a ketogenic diet because, like I said, the ketogenic diet for epilepsy is not the ketogenic diet that people use for weight loss.
It’s a very extreme form of diet, which most patients are not able to tolerate, but it is a treatment for epilepsy and can certainly be tried if patients are up for it. I have some adult patients who are doing a ketogenic diet in addition to their medications.
Being Patient: What type of medications are used with epilepsy? I had a dog with epilepsy, and I remember we had to give her phenobarbital, which I believe is in the barbiturates class of drugs to control epileptic seizures. Is that the kind of drugs that are still prescribed?
Zawar: Phenobarbital is one of the older-generation medications. It is still [used]. Especially when I see some of the older patients who have had epilepsy for 20, 30 years, they will be on phenobarbital. It is still a very effective medication. Some of the patients, especially in the ICU, who have ongoing seizures, which are difficult to control, we may still use phenobarbital or other barbiturates, but now we have so many other options.
Like 20, 30, 40 years ago, phenobarbital was perhaps the only, or like one of the few medications. We have so many seizure medications [now]. We have now 30 plus seizure medications. Some of them are older generations, like phenobarbital. They have more side effects compared to some of the newer generation medications like levetiracetam, which tend to have minimal interaction with other medications.
Every medication has some side effects, but most of these newer-generation medications are better tolerated in terms of side effects and interactions, so we have a wide range of medications now.
Being Patient: I’m guessing you don’t know the answer to this just because medications aren’t tested on dementia patients; there’s not a lot of research on medications and how they interact. Are there different treatments for someone who’s been diagnosed with dementia than someone who has not, who doesn’t have dementia but seizures?
Zawar: Good question. The studies have shown that typically, for older people with epilepsy, this is not about people with dementia, just older people with epilepsy, lamotrigine and gabapentin are considered the first line of medications. Just like you said, seizure medications have perhaps not been studied that extensively in people with dementia, but there are some studies that have suggested that levetiracetam is something that can be tried.
Lamotrigine is another one that has been considered; levetiracetam is typically pretty well tolerated. Sometimes, it can worsen, and it can cause some behavioral side effects. So, for people with dementia, one has to be a little bit more cautious. But the studies that currently exist are mostly about the levetiracetam or lamotrigine used in people with dementia. Again, the use will vary.
At least right now, there is no clinical guideline that tells us that people with seizures and dementia should be treated differently, in turn, than people without dementia. But I would say that we have to, as we move forward, take frailty into account.
Frailty, it basically impacts patients’ tolerability of medications. So, in my practice, typically, I would start patients on a lower dose of medication in people with dementia and go up as tolerated, compared to somebody who wouldn’t have dementia, but it’s just something to consider. In terms of medication choice, I don’t think there’s a huge difference. It’s just the way we start and perhaps go up. That may be slightly different.
Being Patient: What should people know about these types of treatments? What should the expectation be— if you’re on medication, no seizures or an occasional one? Typically, when people start treatment to control the seizures as a neurologist, is your goal zero seizures, or is that not realistic?
Zawar: In general, in epilepsy and seizures, up to 65 to 70 percent of patients become seizure-free on seizure medications. So, if you treat around 100 patients, 65 to 70 people should be completely seizure-free, which is a decent number. Then, there are people who can be very difficult to control the remaining 30 to 35 percent. If they fail to [respond to] medication, we call them drug-resistant epilepsy. They may have to look at other options, including brain surgery to get rid of seizures and those kinds of things.
The good news for older people and people with dementia is that, typically, their epilepsies tend to respond well to medications. My goal as a neurologist will always be to make the patient seizure-free. However, it is really a collaboration between the neurologist and the patient, right?
If they’re not able to tolerate a higher dose of medication, they’re like, “I’m okay with one mild seizure a month, but I don’t want to go up any higher than this.” So, it’s really working between them, but my personal goal is always to make my patients seizure-free— but I have to look at other aspects, including their tolerability of medications and how open they are to consider brain surgery if they’re not responding to medications.
Being Patient: Could repeated seizures actually make cognitive decline worse? If you treat the seizures, does that take care of the cognitive decline? What should people’s expectations be?
Zawar: I don’t know how much the seizures are contributing definitely, but we have seen an association between recurrent seizures compared to remote or resolved seizures. That’s what I was presenting at the American Epilepsy Society. When we compare recurrent seizures in patients to those who have remote or resolved seizures, the time to cognitive decline is much shorter for people with recurrent seizures. So, it does seem like there’s an association between recurrent seizures and accelerated cognitive decline.
Now, we don’t have enough research done in this area for me to tell you if we can reverse it. Typically, if a certain degree of cognitive impairment has occurred, it varies from patient to patient. It depends on how much. Some patients are solely experiencing cognitive impairment because of ongoing seizures. Once their seizures get under control, their cognition may improve significantly, but [if] they also have underlying structures that have gotten significantly impaired in cognition, then it may not improve.
It’s a very case-to-case basis, but there are not enough studies that have been done to show that this accelerated cognitive decline that we are seeing in recurrent seizures, compared to remote or resolved seizures. As an optimist, I would imagine if the recurrent seizures have an association with early cognitive decline, then for me, it’s another reason to get the seizures under control for my patients
Katy Koop is a writer and theater artist based in Raleigh, NC.