The tangled amyloid and tau proteins that accumulate in the aging brains of people with Alzheimer’s have been a major focus for drug developers as well as researchers in recent years. But the inflammation that subsequently flares up in the brain may be an even more important target for researchers developing new drugs to combat the disease.
Researchers from the University of California (UC), Berkeley and Ben-Gurion University are focusing on attacking inflammation as one approach to slowing the effects of neurodegenerative diseases like dementia. In a new study, they found that giving mice with neurodegeneration a drug that fights inflammation improved their brain function and ability to learn new tasks.
An Inflammatory “Fog”
The blood-brain barrier is a wall made up of endothelial cells separating the brain from the rest of the central nervous system. This barrier is semi-permeable, meaning it allows certain molecules to pass through — like glucose and amino acids — but not pathogens or other unhealthy agents.
But as the brain ages, the blood-brain barrier becomes “leakier,” allowing infectious agents to enter the brain and cause inflammation. According to the authors of the latest study, after the age of 70, up to 60 percent of adults end up with “leaky” blood-brain barriers. The aging brain is also more vulnerable to other problems, such as an increased risk of developing tau protein buildup.
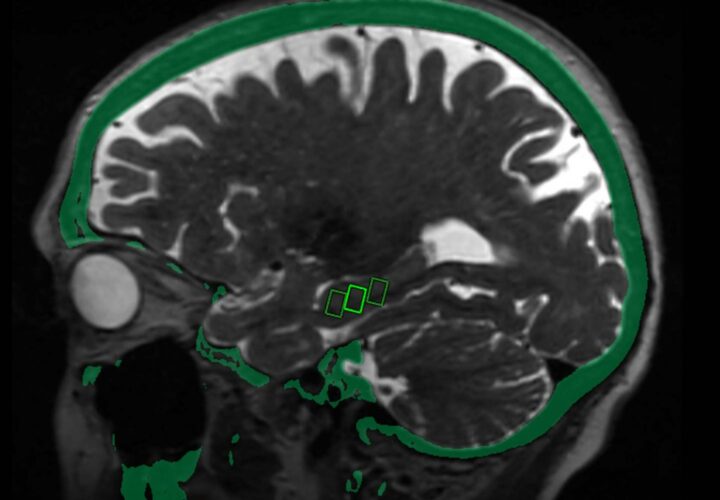
In another paper, researchers found that a leaky blood-brain barrier caused by aging can lead to an “inflammatory fog,” which has shown to impair the brain rhythms of mice in studies. The impaired brain rhythms lead to lapses in the hippocampus, the area most associated with memory and learning — and may contribute to Alzheimer’s disease.
“We tend to think about the aged brain in the same way we think about neurodegeneration: Age involves loss of function and dead cells,” said Daniela Kaufer, a professor of integrative biology at UC Berkeley and a senior author of the study, in a news release. “But our new data tell a different story about why the aged brain is not functioning well: It is because of this ‘fog’ of inflammatory load.”
Fighting Inflammation Through Drug Therapy
In previous research in 2007, Kaufer and co-author Alon Friedman of Ben-Gurion University dug into a certain blood protein known as albumin, which leaks into the brain after traumatic brain injury. Once there, albumin links to astrocytes, TGF-beta receptors in brain cells. This spurs an inflammation response that damages brain cells in a variety of ways, and increases the risk of seizures and epilepsy.
When studying albumin in mice, the researchers found that losartan, a drug for high blood pressure, blocked the TGF-beta receptor in astrocytes and reduced the risk of developing epilepsy.
They decided to further examine albumin’s effects on the brain in the latest study, finding that it was responsible for making young mice brains act much older.
Introducing a drug into the picture, meanwhile, offered some promise for a potential therapy. Developed by Barry Hart, a medicinal chemist in California, the drug — known as IPW — blocked TGF-beta receptor in astrocytes.
When given to mice, IPW lowered the receptor activity level and made aged mice brains appear younger. It also reduced inflammation and boosted brain rhythms, helping the mice perform better on cognitive tasks like going through a maze, as though they were young again.
“When you remove that inflammatory fog, within days the aged brain acts like a young brain,” Kaufer said. “It is a really, really optimistic finding, in terms of the capacity for plasticity that exists in the brain. We can reverse brain aging.”
Though the research will need to be carried out in humans before it can be developed into any clinical use, the researchers note that there are signs of albumin in human aging brains.
In recent research, scientists found that inflammation may actually drive the buildup of amyloid protein in the brain. Finding ways to treat the inflammation may be one path forward in the Alzheimer’s research sphere.