Research into an Alzheimer’s biomarker protein called tau led to a new generation of diagnostic blood tests — and it may lead to new treatments, too.
When neurologists first studied the brains of people with Alzheimer’s, more than 100 years ago, they spotted two abnormal clumps of proteins — beta-amyloid plaques and tau tangles. For decades, scientists focused on studying the role of beta-amyloid proteins in Alzheimer’s because they started to pile up more than a decade before the first symptoms. But in the 1990s, neurologists like Bruce Miller started paying more attention to the role that tau plays in Alzheimer’s and other dementias. In fact, Miller has called it dementia’s “holy grail.”
In Alzheimer’s, tau proteins, which usually help stabilize neurons in the brain,start getting tangled up, damaging and killing off brain cells.
Measuring the levels of tau pathology inside the brain is now thought to drive the trajectory of cognitive decline more than beta-amyloid. Better yet, the levels of tau biomarkers in the blood and brain are also good predictors of beta-amyloid plaques. Tau proteins are measured by the newest and most accurate blood tests for Alzheimer’s, and targeting them may be key to finding the next treatment.
Measuring tau to diagnose and monitor Alzheimer’s disease
Many researchers and drug companies are using tau PET scans in clinical trials to identify patients who might benefit from a new drug. Tau PET scans can also give clinicians more certainty over a diagnosis—many dementias have overlapping symptoms, and getting the right diagnosis is key to finding the right treatment for the individual.
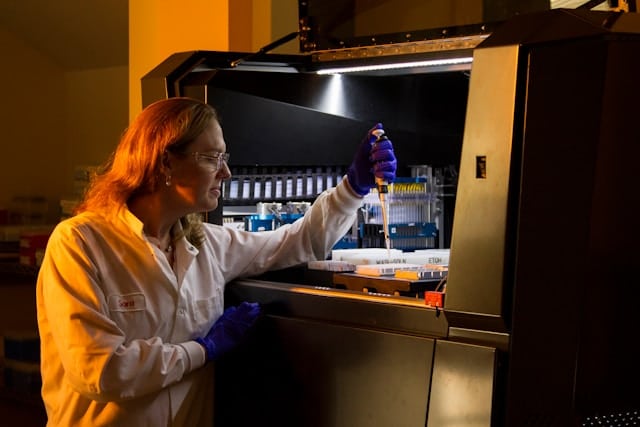
But PET scans are only available in large hospitals and research universities, making them hard to access for many in the US. Fortunately, blood tests might be able to accurately predict the levels of tau and amyloid in the brain at a lower cost.
Many of these tests look for pieces of tau that have made it from the brain into the bloodstream to help a doctor rule in or rule out Alzheimer’s. Some of these tests can perform as well as a cerebrospinal fluid test or amyloid PET scan, making them less invasive for patients.
Biologics: Anti-tau antibodies and tau vaccines
Anti-tau antibodies
Several drug companies are developing anti-tau monoclonal antibodies.
There’s already one Alzheimer’s monoclonal antibody on the market called Leqembi, which targets amyloid proteins, rather than tau proteins, but these drugs cause ARIA — brain swelling and brain bleeds — a risk which some neurologists argue outweighs the benefits of the treatment.
But there’s good news about anti-tau antibodies: They don’t cause ARIA like their anti-amyloid counterparts.
So far, two new monoclonal antibodies targeting tau have gone through a preliminary Phase 1 trial. Jannsen is currently running a Phase 2 trial of its anti-tau antibody JNJ-63733657 in early Alzheimer’s disease, slated to end in 2025. Drug company Prothena is also developing anti-tau antibodies and recently licensed PRX005 to Bristol Myers Squibb, which will conduct a Phase 2 trial in the near future (the company hasn’t announced yet when the trial will start, but sign up for Being Patient Trial Updates newsletter to stay up to date).
Tau vaccines
Vaccines help train the immune system to recognize and clear out misfolded tau proteins.
Last year, Axon Neuroscience presented phase 2 trial data of its tau vaccine AADvac1. The overall results weren’t positive, as the vaccine didn’t slow cognitive decline. However, analysis after the trial revealed that some patients with high levels of amyloid or tau may respond to the treatment, but more trials are needed.
Small molecule drugs: Pills to stop tau in its tracks
Several companies are developing small-molecule drugs that target tau. A treatment in pill form would be cheaper than monoclonal antibodies and would not require patients to travel to an infusion center or doctor’s office for treatment.
TauRx has been working on a drug called hydromethylthionine mesylate (HMTM), which prevents the formation of tau tangles (which is what damages and kills brain cells.) While the drug has failed several Phase 3 trials so far, and experts have been highly critical of the results, the drugmaker is hoping it might still work and is in talks with U.S. regulators about filing for approval based on the data.
Annovis Bio is currently completing its phase 2/3 clinical trials of buntanetap, a drug that prevents the formation of toxic proteins in the brain like tau, amyloid, and TDP-43. The drug is being tested for treating patients in the early and moderate stages of Alzheimer’s and Parkinson’s disease. The company also plans to test its drug in the later stages of dementia.
Thanks to research into tau proteins, new blood tests and tools help doctors make an accurate diagnosis, and with drugmakers also focusing on this protein, it’s possible that one of the next drugs approved for treating Alzheimer’s will target tau instead of amyloid.




Thank you for posting this article! It gives those of us who are children of Alzheimer’s patients hope for the future.
Thank you for being here, Sheri!
Regarding drug trials and new potential treatments for tau tangles, Biogen is currently in Phase 2 of testing a new drug that goes after the tau. My husband is in their drug trial through NYU Langone Hospital in NYC. This study is nationwide.
Thank you for participating in these trials, Madeline! Please keep us updated on your husbands progress. Take care.
#Biogen’s #Gosuranemab #BIIB092 was extremely helpful in treating my husband’s #attypical #parkinsonism #corticobasal syndrome. Unfortunately the drug is not manufactured anymore. It reduced tau by 97% in his spinal fluid.