Hardly a week goes by when I don’t receive an email or a call from a friend whose parent has just gotten an Alzheimer’s diagnosis. This past week, I heard from a close friend and her sister, who called to ask for my opinion about what they should do. Their mom had just been diagnosed with an early stage of Alzheimer’s disease.
My friend sent me her mom’s official diagnosis which made the following points:
- The score for her MMSE cognitive test was in the “possible early Alzheimer’s” range.
- The doctor didn’t feel that neuro-imaging was necessary, because, as the doctor wrote, “This rarely changes anything.”
- The patient was prescribed Aricept and told to see how she tolerated it before increasing the dosage.
- And lastly, the daughters were told to “investigate possible memory care units.”
This, readers, is a prime example of what has gone terribly wrong in many neurology practices — and unfortunately, this is not an uncommon experience for people.
Based on what I have learned from interviewing hundreds of medical experts, researchers, and patients, coupled with our team of journalists’ excellent reporting, here was the advice I gave to my friend:
1. Ask for a blood biomarker test.
Alzheimer’s is frequently misdiagnosed. To make sure they’re right, doctors should be gathering all the information they can get. Alzheimer’s has two key biomarker proteins that clump or tangle in the brain: beta-amyloid and tau. In the past year, several blood tests have hit the market that test for these biomarkers in the blood stream. They can’t diagnose Alzheimer’s on their own, but they can certainly help confirm a diagnosis. So, if you get an Alzheimer’s diagnosis based on a cognitive test, ask your neurologist to order a blood biomarker test to confirm there is actually amyloid in the brain. (Specifically, consider the blood tests that measure PTAU271, the biomarker several neurologists have told me is the most accurate.)
2. Consider new disease-modifying Alzheimer’s drugs.
If the blood test results come back in the “high risk” range, arrange for a PET scan to see if the person diagnosed is a good candidate for either of the two monoclonal antibody (mab) drugs newly approved by the FDA (Kisunla and Leqembi). Medicare has now approved one PET scan for likely candidates for these mab drugs. I cautioned my friend that these drugs are not for everyone, especially if her mother is a carrier of the genetic variant ApoE4, as this variant indicates a higher risk of side effects on mab drugs, namely ARIA (brain bleeds or swelling).
I also suggested that her family may want to consider genetic testing if it looks like amyloid is present — but that is a conversation they must have as a family. (As Doris Zallen, author of “To Test or Not to Test” explained well in one of our Being Patient Brain Talks, this path isn’t for everyone.)
3. Get confident about the diagnosis.
If amyloid is not present, inquire about other dementias. We talk to people regularly who lived for years with an inaccurate diagnosis. In this case, the neurologist report stated that there were signs of tremors in one hand. My question would have been: Why are they eliminating Lewy body dementia? (Being Patient has interactive learning guides for all of the most common dementias to help patients better understand their diagnosis.)
4. Prepare for the future — but don’t fast-forward to it.
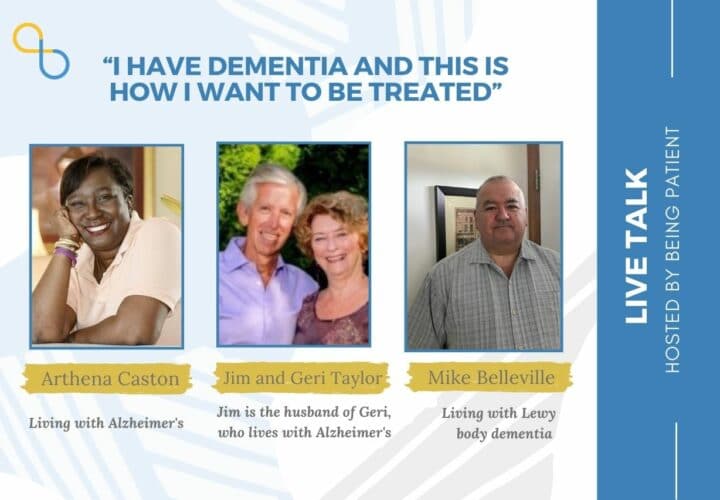
Also: Why is this family being told by a neurologist to look for memory care homes at this very early stage? Many people with a diagnosis have told us nothing makes them more angry than being told to get their affairs in order. That message sends a chilling sign that it is the beginning of the end. Being Patient has heard endless stories from our patient community of reinventing life through the arts (Alzheimer’s doesn’t diminish the brain’s capacity for creativity — that’s why people discover artistic talent or don’t forget a musical instrument until the very end stage), or setting ambitious goals to test resilience that are truly inspiring! So many of the people we talk to are far from needing to live in a long-term care home: They’re climbing mountains, writing memoirs, and speaking at the UN.
5. Make science-backed lifestyle modifications.
Why wasn’t a program for science-backed, brain-healthy lifestyle habits prescribed, with a lot of social engagement, which is proven to protect brain health and shown to, for some people, help slow symptoms? As Dr. Claudia Kawas told me in this Brain Talk about super-agers, the one commonality in the 90-plus study with people who did have Alzheimer’s biomarker amyloid in their brains but who didn’t get Alzheimer’s symptoms? Eight hours of social engagement per day!
6. Identify and treat health issues that mess with cognitive function.
Along with the neurologist’s cognitive test, why wasn’t a blood test ordered to look for deficiencies, like vitamin B12, D and metal toxicity or a urinary track infection, which can have a significant impact on cognition? While dementia isn’t reversible, its precursor mild cognitive impairment — depending on its underlying cause — may be! (Learn more about MCI’s treatable causes right here.)
7. Include mom in the conversation.
Most importantly, I told this family they should involve their mom in the conversation about what matters to her. Give her a choice on matters going forward, rather than dictating what they think is best. I learned this first-hand with my own mother, whom we drove to tears for talking around her, almost as if she wasn’t present in matters she had always been responsible for.
I still feel remorseful today for how we handled the initial conversation back then — because no one had told me that just because someone is living with Alzheimer’s-related memory loss, it doesn’t mean that they don’t feel emotions that stay with them, even into very late stages of the disease.
***
This journey isn’t an easy one. But I also believe it doesn’t need to be as difficult and daunting as a diagnosis may seem — not when a family is empowered with the right information. A loss of memory doesn’t mean that people cannot feel useful anymore. Alzheimer’s doesn’t mean that you cannot accomplish new things — even begin an unimaginably fulfilling new chapter of your life. It just means you need to figure out a new pathway for a different type of life. That starts with knowledge. I only wish more neurologists could provide it.
‘I’m the Very Same Person You Knew Before:’ How To Talk to a Person With Dementia


I think your 8 points that you offer for what to do after a diagnosis are great, however #5 seems to be missing?
Hi Lori, thank you for noting this. We’ve updated it on our site. Take care!
Great article, but what happened to Number 5. I’m far from being a smart Alec, just curious. The other 7 points are pertinent and relevant.
Hi David, we’ve now updated the article. Take care!
Thank you for shedding light on the common missteps in Alzheimer’s diagnosis—it’s crucial to ensure patients feel heard and understood. At Pavan Neuro Center (www.pavanneurocenter.com/neurological-health-matters.html), we prioritize personalized care and empowering individuals through accurate diagnoses and comprehensive support.
Hi there, thank you for the work you’re doing at Pavan Neuro Center. Accurate diagnosis and patient-centered care are essential. We’re grateful to have you as part of the Being Patient community.