Following the approval of the Alzheimer's drug Aduhelm, one question that's top of mind for patients is: Does Aduhelm work?
Following the approval of the Alzheimer’s drug Aduhelm — and the litany of controversy surrounding it — one question that’s top of mind for patients is: Does Aduhelm work? Being Patient speaks to trial participants and clinical recipients of Aduhelm, the first Alzheimer’s disease-modifying drug ever, and the first Alzheimer’s drug of any kind to be approved by the FDA in nearly two decades.
The Food and Drug Administration’s approval of the new Alzheimer’s drug Aduhelm (aducanumab) was a landmark decision, one that has also sparked major controversy in the Alzheimer’s community. Some experts have hailed the approval of the drug — the first-of-its-kind to be green-lit by the FDA — as the start of a new era of Alzheimer’s treatments. But others have criticized the FDA, saying the agency approved the drug prematurely given that Aduhelm’s efficacy remains unclear. In the aftermath, several hospitals and health centers have declined to administer the drug. Some insurers have said they won’t cover it. And sales of Aduhelm, which costs each patient some $56,000 annually, have fallen short of expectations so far. This has all left Alzheimer’s patients and their families wondering: Does Aduhelm work? Can it slow the progression of Alzheimer’s?
Some trial participants believe the drug has seemed to help preserve their independence, at least to a certain extent.
About three years after her diagnosis of mild cognitive impairment, Geri Taylor enrolled in a clinical trial of Aduhelm in 2015. Her husband Jim Taylor noted that she declined very slowly before the trial was halted.
“We really thought the drug was helping,” Jim told Being Patient. “Of course, there’s no way to know that, but her ability to maintain normal daily activities and live and take care of herself was really excellent. We traveled all the time and she managed all that well.”
But in March 2019, Biogen and its partner Eisai terminated the two Phase 3 trials of Aduhelm, following an interim analysis that showed the trials were unlikely to meet their main objective: slowing cognitive and functional impairment of patients with early-stage Alzheimer’s. It was devastating news for the Alzheimer’s community, including families and trial participants like Geri and Jim. After Geri and her fellow participants were taken off of the treatment, her condition progressed faster than before, Jim said.
Then, in October 2019, the rollercoaster ride for Aduhelm trial participants took a new turn: Biogen and Eisai showed that in a new analysis, the drug appeared to slightly slow the decline of patients who received the highest dose of the drug in one trial. The other trial failed to show any benefit. Since then, the drugmakers have relaunched clinical trials, and Geri has been receiving monthly infusions of the drug again. But Jim theorizes that the window of opportunity for effective treatment has passed.
“During what I call the interregnum, the period when she wasn’t getting the medication, she started to decline more quickly,” he said. “Now that she’s back on the drug, I kind of doubt it’s helpful. The benefit is really to get started as early as possible.”
When asked “Does Aduhelm work?,” trial participant, Phil Gutis, thinks the drug has benefitted him in some ways, too: “Anecdotally, I believe that aducanumab has helped me,” Gutis, who is a Being Patient reporter, wrote in a reflection of Aduhelm’s trials and his diagnosis of early-onset Alzheimer’s about five years on. “I feel much better than I did five years ago. Truthfully, five years ago, I didn’t expect to still be alive today.”
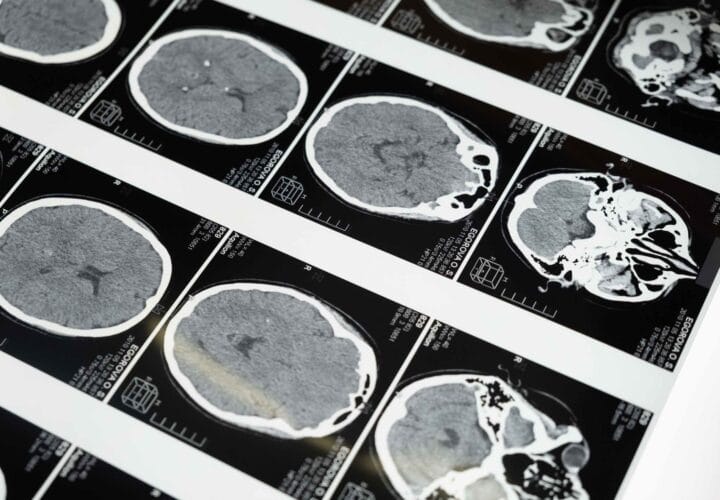
While available medications can treat Alzheimer’s symptoms, Aduhelm is the first FDA-approved Alzheimer’s drug that addresses the underlying disease. The monoclonal antibody is designed to stimulate the immune system to remove amyloid plaques, accumulations of misfolded proteins that are found in the brains of people living with Alzheimer’s.
From a longitudinal study’s brain imaging results, Gutis learned that these plaques are no longer present in his brain. He described feeling like “emerging from a constant mental fog,” but added that his memories of daily events, whether it be going to comedy shows, restaurants, theaters, or hiking at the quarry, continues to fail him regularly.
“The memories that I’ve lost have not returned,” he said, “and I continue to stumble across activities that seemingly were never written into my memory banks.”
The only effective dose of Aduhelm, if at all, seems to be the highest dose. Clinicians increase the dose over time to reduce the risk of side effects. So, Marc Archambault, who received his first infusion of the drug in June, said it’s too early to tell whether Aduhelm has slowed the progression of his disease. Since June, he has been receiving monthly infusions of the drug, and Archambault, diagnosed with early-onset Alzheimer’s, has hope that Aduhelm will help him and others.
“I was very lucky and very happy,” Archambault, who was the first patient to be treated with Aduhelm outside of clinical trials, told Being Patient of the day he received his first infusion of the drug. “I was ready to take it. I’d been reading about it and I thought I’d be crazy not to take this, never mind I was the first person.”
“It was on all the news that night in Rhode Island and Boston and it was amazing,” he added. “That part was kind of fun. People said, ‘Wow, you’re famous.’ I said, ‘I think it’s the drug.’”
Aduhelm, like any drug, carries risks for patients. Chief among these for Aduhelm are side effects of brain bleeding and swelling, known as amyloid-related imaging abnormalities (ARIAs). For trial participants who were treated with the highest dose of the drug, the vast majority of ARIAs were asymptomatic, and symptomatic cases were rarely severe.
Former Aduhelm trial participant Daniel Gibbs experienced ARIA first-hand, and in fact, as clinicians in an Aduhelm trial were ramping up doses of the drug for Gibbs, he had a rare, extreme experience with this side effect. Gibbs recalls a series of increasingly severe headaches accompanied by cognitive issues. Through magnetic resonance imaging, doctors determined that Gibbs was experiencing ARIA, and he recovered following treatment with steroids.
“It took about six months for the swelling in my brain to totally go away,” Gibbs, author of A Tattoo on My Brain, told Being Patient. “The little spots of hemorrhage interestingly are still there and that gave me the title for the book. It’s the tattoo on my brain, that little bit of iron-containing pigment.”
While the severity of his experience was an outlier, ARIAs occurred in more than one third of patients treated with the highest dose of Aduhelm during clinical trials, and some experts believe it’s not worth the risk of potentially serious side effects given that Aduhelm’s benefits for patients are unclear and at best, marginal.
But the FDA based its approval on the drug’s ability to clear amyloid plaques, which the agency believes “is reasonably likely to predict a clinical benefit to patients.” The move went against objections from an independent committee that overwhelming rejected evidence of Aduhelm’s efficacy in November 2020. In protest against the decision, three members of the committee resigned (one of them had recused himself from the November meeting as he had been a site investigator of an Aduhelm trial).
According to Dr. Lon Schneider, director of the California Alzheimer’s Disease Center at the University of Southern California and former site investigator of an Aduhelm clinical trial, the drug is clearly effective at flushing out these plaques, but there isn’t sufficient evidence to show that it can in turn actually slow patients’ decline.
“We have a drug that’s approved to decrease that biomarker — those plaques — and we have a good amount of uncertainty about ultimate benefits,” Schneider told Being Patient. “That comes back to the uncertainty of the approval indication.”
Before Aduhelm, scientists have developed therapies that can effectively clear the build-up of amyloid as well, but these experimental drugs have largely failed to show any benefits for patients. In the case of Aduhelm, Biogen is required by the FDA to carry out a post-approval study, and the drugmaker, along with Eisai, have announced plans for a Phase 4, observational study to examine Aduhelm’s safety and effectiveness in clinical practice.
Image: Aduhelm, Biogen/AP.





do the above statements also apply to the 3D phase trial by Elly Lilly on Donanemab?
I am a patient in the clinical trial.